 Dr. Lynsey Bartlett made national news when she let 100 patients go last week. CTV reported it as 200.
Dr. Lynsey Bartlett made national news when she let 100 patients go last week. CTV reported it as 200.
She was charting until midnight, spending 1/3 of her day with complex mental health patients and could not afford to hire more staff to help out.
She was simply overwhelmed.
Many docs do what Bartlett did, but they go quietly. They trim office hours or join larger groups.
Patients wait longer for next-available appointments. But no one sees it in the news. Access changes like the tide, quiet and slow.
The tide has shifted, in Ontario. Ten years ago, doctors had hope. Federal Health Transfers filled provincial coffers. The economy roared, and healthcare funding rebounded, after 10 years of social contract cuts.
But hope has worn thin lately. The 2008 financial crisis hit government revenue. Doctors have been attacked on all fronts. Spending now goes mostly to unbeatable interests; austerity does not win elections.
Overwhelmed
Medicine is not what it used to be.
A UK study reports 2/3 of docs wouldn’t recommend a career in medicine to their children. American docs are burning out at alarming rates.
In Canada, some studies report up to 75% of trainees are burned out, and 50% of practicing physicians show signs of burnout. The Canadian Medical Association reported that 26% of doctors are dissatisfied with their work life balance.
On top of this, Canadian doctors commit suicide at a rate 2-3 times the general population.
Politicians, journalists and academics usually blame aging patients and burden of care:
Older Patients – The average Canadian was 25 years old when Medicare started. People hoped to live until 70.
Today, life expectancy for women is 84 and for men it’s 80. The average Canadian is over 40. As of 2017, Canada has more seniors than children.
Demography crushes clinical care. Old people need the most care, ergo, even a tiny change in the number of seniors creates a massive change in total care.
Sicker Patients – Medicine used to be about diagnosing with limited tools and treating with limited therapies.
Today, physicians sift through long lists of medications, trying to figure out whether symptoms represent disease or side effects.
Docs used to diagnose and treat. Today, they educate and motivate.
But older patients are fun. They give rich past medical histories and do not take themselves so seriously. Sick patients define why doctors became doctors. Neither old nor sick patients fully explain why doctors are overwhelmed.
Insufficient Resources –
Dr. Bartlett mentioned how hard it was to care for really sick patients without specialist backup. She was seeing some patients twice weekly until a specialist could take over.
“I was not trained for this. I am doing my best, but there are just not enough resources in the system.”
She extended office hours to keep up with demand, but it’s not enough.
It’s the same everywhere. Patients languish in hallways waiting for a hospital bed. Families care for relatives at home for years after patients should have been in long-term care.
Too Much Regulation –
Since 1970, health regulation has exploded in Ontario (see graph).
Regulation means doctors spend more time thinking about following rules than listening to patients.
Each law expands the size and power of government.
For example, Bill 160, a 200 page omnibus bill, amends or introduces 10 different pieces of healthcare legislation. It gives government broad powers but offers few details about scope or intent.
The bill introduces oversight to ‘healthcare facilities’ but does not define a facility. Without definition, every single doctor’s office might be considered a facility and be open to oversight by an external administrator.
This is just one problem in one bill. Businesses in Ontario already face 380,000 regulations, and yet governments put more and more responsibility on doctors but give MDs less and less control.
Increasing Expectations –
Patients expect more, and who can blame them? If a laptop doesn’t turn on in 2 seconds, we wonder if it’s broken.
Medicine, for the most part, has not kept pace. Doctors still rely on fax machines (!). We make people wait in waiting rooms.
Regulatory colleges demand long clinical notes that list all the symptoms a patient did NOT have just to prove that the doctor thought about all the scary things that did not exist.
As patients expect faster service, a sticky mass of bloated administrative duties threatens to smother doctors.
Not Enough Time –
Today, doctors must run faster to pay for overhead and maintain a reasonable income.
Some people hate talk about fees and wish fees did not exist. They push salaries. But governments cannot afford to put all doctors on salary. Salaries have their own challenges, starting with misaligned incentives and lower productivity.
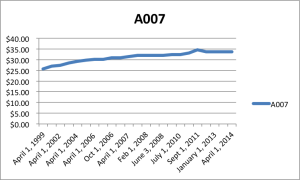
Fees have remained flat or declining for years (see graph).
Falling prices – fees in this case – cause businesses to act in predictable ways.
When prices fall and overhead increases, businesses must trim products and services. Bakeries bake shorter loaves of bread and mechanics spend less time chatting with owners.
Cuts force doctors to trim clinic visits as short as possible, and doctors get blamed for the experience.
Eroded Respect –
Many doctors went into medicine to help people and earn respect for helping. Who could imagine a better career?
In single-payer healthcare, the only thing people talk about is money, and how there’s not enough for everyone who wants it.
Governments spend most of their healthcare dollars on hospitals and doctors’ fees. As money runs out, hospitals and doctors become targets. With less funding, hospitals leave patients in hallways and doctors change the way they practice.
If bakeries sold shorter loaves because government reduced the price of bread, bakers would get blamed. Few people think about the price-fixing and regulations that caused it.
Overall, nationalized services tend to create frustration at the point of service, not respect.
Overwhelmed but Grateful
Most doctors hold on to inspiring stories: the ones where patients benefit and doctors become better people.
I had a long talk with Dr. Bartlett. She has a passion for sick patients. She agonized over her decision. She made sure that her 200 patients were stable: none of them had major mental health or medical issues. Many lived in another city.
We talked about the media camped outside her office. She giggled about trying to wait until they left. Docs just want to care for patients. They aren’t trained to handle reporters.
We need more doctors like Dr. Bartlett. She welcomes the sickest. She stays late and cares deeply. She extends her office hours, but she also knows her limits. Trying to save the world is risky, not heroic.
Many doctors are overwhelmed. Our system needs a new approach. We cannot just talk about money and fees.
We need to talk about regulations and incentives. We need to unleash innovation and allow failed programs to die. We need to talk about society and politics, and try to figure out what voters want.
If we do not improve things soon, doctors who are simply overwhelmed will be forced to change or quit. It doesn’t need to be like this.
Addendum: A few days later, Dr. Bartlett let me know that she had only let 40 patients go, and might only hit 75 total.
Photo credit: MetroNews


Excellent comments and analogies, Shawn! Most docs haven’t seen these graphs before, and I think those, and similar such graphs and visual aids should be sent out to physicians. We should create posters for our exam rooms. A great one would be the average time-spent-with-patients shift that has occurred over the past 20 years. And the average amount of time spent on charting over the last 40 years. I bet that it would mirror the regulations graph. What about a graph showing patient illness in some fashion. I suspect there is an inverse relationship between the.severity of illness vs the amount of time taken to see patients. Keep us thinking.
You hit a lot of nails right on the head here, Shawn.
I would like you to read what the College of Physicians and Surgeons of BC is expecting doctors to do when prescribing narcotics. I would not have a single minute to practice medicine.
And something has to be done about the regulating bodies. They got too comfy, no stress, renting huge downtown 5 stories spaces – for who?
Thank you for writing this post. I’ve been a silent follower of your blog for years, feeling bolstered by your reflections and insights.
I have been a full-time emergency physician for over ten years. In the last few I have realized that this career is not sustainable for me. Your post outlines the reasons very well. I often tell the residents that I teach, “You might think the hardest part of medicine will be not knowing what to do. It’s not. It’s knowing what to do and not being able to do it.” Constantly struggling and engaging in conflict (with the system, hospital, even colleagues sometimes) just to do right by our patients will wear anyone down.
Like a handful of other physicians, in order to understand my experience I started a little blog not long ago. One of my first posts is about physician burnout. I will add the URL below. Not self-promotion. I hope that my words are worth reading, but the comments certainly are. Amazing insights and heartbreaking stories.
A sincere thank you for your thoughtful leadership.
Not sure if the link worked . . .
http://better-than-normal.com/2017/10/31/burnout-the-new-normal-for-doctors/
It is painful to read what our healthcare system has done to our physicians. 😪
“Knowing what to do and not being able to do it”. Well said. We must come to terms with what we are humanly able to do and accept that while working on solutions TOGETHER. Conversations and awareness are the beginning. We must continue these conversations with all those involved, not just those of like mind. Thank you Matt for your added voice.
Thank you Shawn! Very precise. It’s time to start making some very unpopular choices. Only then will things start changing for the better.
Why can’t you put your blog on the OMA site and release it to the media ?
MANY good pots….
However,we can’t avoid looking at funding of the system and getting more (private) money in like France for eg …. can’t stick our head in the sand.We owe it to DOCTORS.
Why can’t you put your blog on the OMA site and release it to the media ?
MANY good points….
However,we can’t avoid looking at funding of the system and getting more (private) money in like France for eg …. can’t stick our head in the sand.We owe it to DOCTORS and PATIENTS.
Over my 40 years as a physician I have seen and felt these changes. Your reflections on Dr. Bartlett’s experience, and the comments which follow resonate strongly with my own. Thank you for your leadership in identifying what’s not working and thinking harder about what could be.
Shawn, you are correct.
However, physicians need to take back control not wait for it to be given to them.
This can happens with a request from our OMA president for targeted action from all physicians at the same time. For example, if we were all asked by you to do the same thing that Dr. Bartlett had the courage to do on her own at the same time, these issues you raised would have to be dealt with. If this was done and coupled with the solution for system inefficiencies tied to economic barriers, the system and patients would get the overhaul you are asking for.
Unfortunately, this is what is missing from the OMA’s actions (or a lack of solutions to be targeted and implemented) as the system, physicians and patients continue to suffer.
This ongoing deficiency is creating a slow change in the system that is not necessarily better for anyone. This is job change and we are living it, experiencing it, and not targeting the cure together as Dr. Bartlett has so bravely done on her own.
So I leave you with the question on everyone’s mind, when will we take these actions together to create a better system that you speak of.
Regards,
Dr. A
From the NYT (I think today) https://www.nytimes.com/2017/11/13/well/family/taking-care-of-the-physician.html
Thanks for this. I spent my life billing A007 for the last 35 years. And it takes more time just to earn that small amount. I have learned 2 computer systems. I now do the work of nurses and receptionists. I email pts all their results. I have had to keep upgrading my skills at my cost.
I have now cut down on the number of patients I see in an hour to 3 because I cannot get all the paperwork done. I spend at least 25% of my time doing charting . I am close to retirement and it is only the love of the profession that keeps my here but I know that the CPSO will be on my heels to get rid of me as I hit 70 soon so I am getting ready to go. It has been a financial loss to have this career and to end it with the governments hitting us from all sides is demeaning and criminal. To have them in our pockets every month right now is beyond belief. My heart goes out to all my colleagues since like the poor doctor above, they are all struggling.
Thank you for highlighting this issue, Shawn.
What shall we do about it?
Terry McQuiston