Schedulers think in LEGO blocks. They guess how much work an average staff member can do, and then schedule enough staff to meet the average amount of work each day.
To build a schedule, they plug staff into a grid, like identical LEGO blocks, to meet the demands of an average day.
4 problems with LEGO block scheduling:
1. Nobody is average.
2. No day is average.
3. Under-staffing makes patients wait.
4. Over-staffing makes costs go up.
Average doesn’t exist in clinical medicine.
Treatment protocols can be standardized, but the core of clinical medicine – history taking and physical examination – remains messy, relational and often intuitive. Ask any emergency nurse: every doctor works at a different speed – same goes for the nurses.
Discussing speed makes most providers squirm. Slow providers say fast ones are slipshod and careless; fast providers say slow ones are lazy or talk too much.
Schedulers run from this time bomb. It’s safer to assume average work speed, and hope that patients won’t wait, and costs won’t soar.
But patients wait… and costs soar.
How can this be resolved?
Let’s look at physician schedules. First, we must re-frame provider ‘speed’ – defuse the time bomb. Dr. Marko Duic put it something like this:
“Every physician has a number stamped on his/her forehead that states the number of patients he/she can safely see per hour. Everyone can see the number, but no one can see his/her own number. Ask any nurse how many patients a physician sees in an hour, and they will tell you as accurately as reading a number off the doctor’s forehead.”
We can’t change the speed people work, and we must welcome every worker onto the schedule regardless of how fast or slow they work.
How can we build a schedule that minimizes patient waits AND maximizes staff efficiency? Furthermore, how can you get staff to want such a schedule?
If you want to schedule for waits AND efficiency:
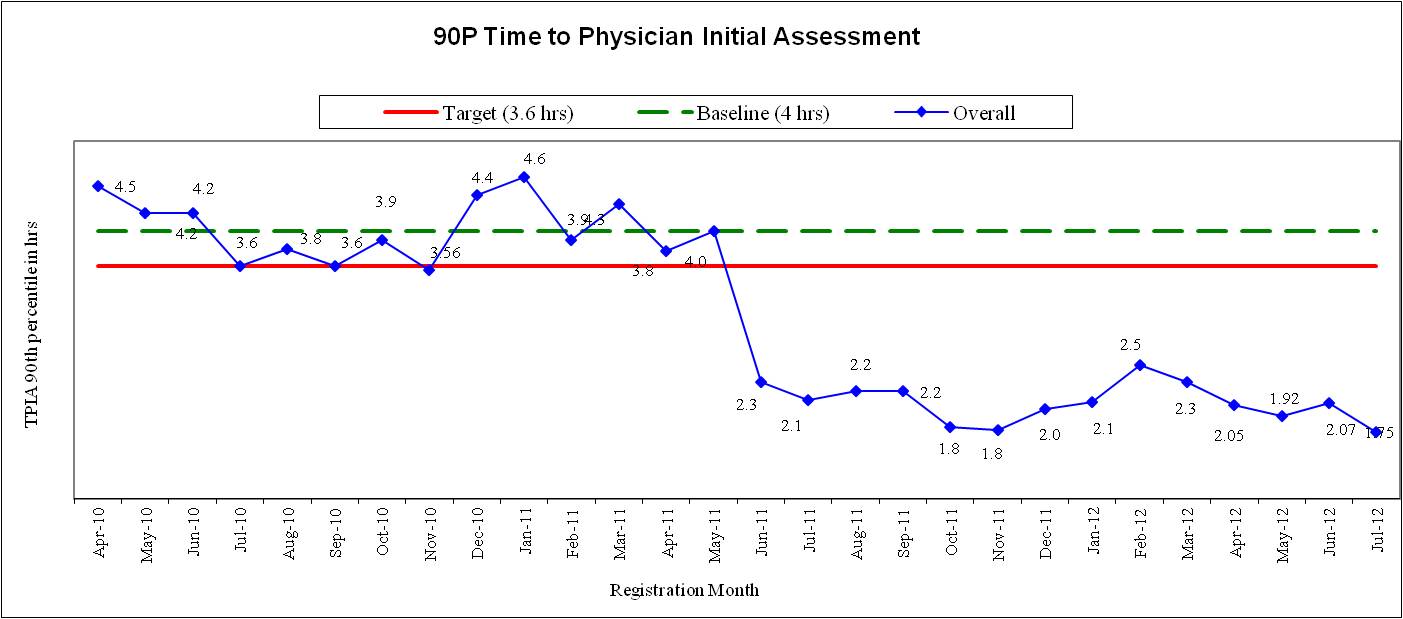
1. You must match demand with productivity. You should know how many patients attend your ED per hour. You know how fast your docs work. Schedule enough MDs, based on their individual work speeds, to meet the average patient volumes by hour. Some days you may need twice as many doctors, if they all happen to be slower on one day.
2. You need hour to hour flexibility. Physicians must stay late, arrive early, go home early or call in more MDs for help when patient volumes warrant. Let the physicians on duty control these decisions, and keep them accountable for the outcomes.
3. You should let physicians chose whatever shifts they want. Choice makes doctors happy. Collect their shift preferences and have them indicate 50% more shifts than they want for whatever time frame you are scheduling (e.g., 1 month). Juggle the MD lineup each day based on #1 above.
We will interview the provincial guru on MD scheduling, Dr. Marko Duic, in one of the next posts to bring out the details.