Some people do not have time to read books. But they listen to podcasts.
Some people do not have time to read books. But they listen to podcasts.
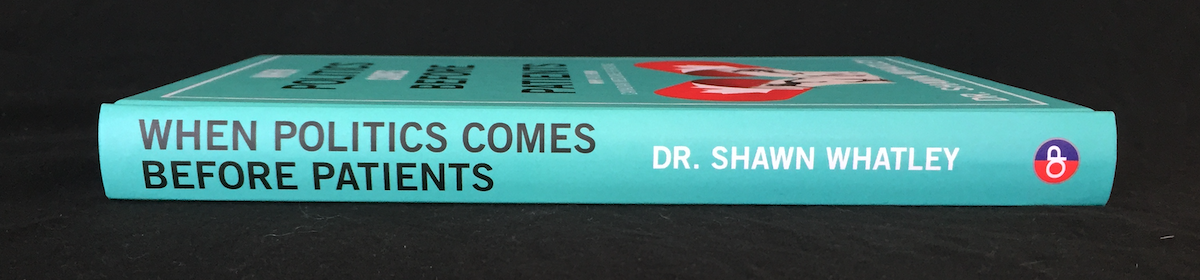
So, I plan to give away as much of the content in No More Lethal Waits: 10 Steps to Transform Canada’s Emergency Departments as I can squeeze into podcasts and short blogs.
The first podcast covers the Introduction and first chapter: Step 1 – Revamp Triage. This blog gives a snapshot and overlaps the podcast. I hope it gets people talking about the ideas, even if they do not have time to read the book.
Here’s the first podcast (I had fun making it!):
Introduction
Doctors, nurses, allied health providers, administrators make patients wait. We blame problems outside our department or clinic. But if we wait for outside help, nothing will improve.
We need to change how we work, first. We have to tackle misaligned incentives, arcane policies, and draconian legislation to do what is right for our patients. We need relentless devotion to improving patient service and care. Even if we only make small improvements, we will have much more credibility when we ask for bigger, system-level, changes.
NMLW uses old ideas. It does not describe a new fad or secret recipe to reform healthcare. We need a new perspective, not another wunder-plan that promises to fix everything.
The ideas in NMLW work together. You cannot close your waiting room without changing nursing ratios, doctors’ schedules, and furniture inside the ED.
If you give these ideas an honest try, you can expect that patients will:
- Not wait in the waiting room
- Be seen by an MD in < 1 hour
- Have the shortest possible length of stay
- Receive the highest quality care and service
Be careful, political responsibility, or system guilt, will ruin your best efforts to improve patient service. We need to put aside our angst about costs, the broader system, and spending for a moment. Only a relentless devotion to patient service will improve ED function.
Devotion to patient service drives down costs per case, length of stay, adverse events, and, in fact, everything in an ED functions better when we focus on patients first, and the broader system benefits for it. But do not start with system guilt; start with patients first.
Revamp Triage
Patient go the ED to get a diagnosis and treatment in the shortest time possible. They have no chance of getting what they need, while sitting in a waiting room.
Triage has become such a part of emergency medicine that we believe every patient deserves a good thorough triaging. Even with doctors and nurses standing ready to see patients, we still force patients through a fulsome triage.
Napoleon’s surgeon invented triage as the army ran out of soldiers. He needed a way to pick out wounded infantry that could be patched up and sent back into battle as quickly as possible.
We invented modern triage as our system started running out of money. Cash-strapped hospitals use EDs as an extra ward, and waiting rooms as overflow. Triage is designed to manage the crowds.
The Canadian Association of Emergency Physicians states that triage, in its simplest terms, is sorting or prioritizing. There has always been some kind of triage, long before modern triage existed. ED registration clerks working alone, out front, on overnight shifts, used to bring in patients who looked too sick to register.
Today, formal triage includes collecting a chief complaint, acuity score, and deciding on the best location for a patient to go. But it also includes a history, screening for influenza-like-illness, a focussed physical, past medical history, medication reconciliation, and a whole bunch of other duties. Large hospitals often employ 4 triage nurses to manage packed departments.
Patients just want a diagnosis and treatment as efficiently as possible. They do not go to the ED to endure processes of questionable benefit. Triage needs to change.
Patient Flow
Most of the time, providers inhibit patient flow. We batch tasks, work inefficiently, or we just get overwhelmed and slow down. Decreased patient flow causes increased length of stay which results in increased workload. There is no excuse for people doing “a really good job” by spending 45 minutes educating one patient, while everyone else waits for care.
At the same time, we cannot confuse great flow with cutting corners, going really fast, and providing inadequate, low quality service and care. We need to do fast things fast and slow things slow.
The Institute for Clinical Evaluative Sciences outlined quality indicators for emergency care. They found evidence for 48 indicators: 23 are related to time, and 16 are entirely time-based, e.g., time to antibiotics, time to ECG, or time to thrombolysis.
For emergency care, time equals quality. In other settings, “quality” balances effective, safe, patient-centred, timely, efficient, and equitable care. But the ED is different.
No matter how ‘great’ care you provide when patients finally receive it, if you make patients wait for hours, by definition, you deliver low quality care.
Historic Triage
We need to triage patients IN to the department and not back OUT to the waiting room. A skilled nurse can collect a chief complaint, assign an acuity score, and decide on the best location for a patient in 1-2 minutes. The rest of of the triage nurses can work inside the department providing care.
That leads us to the next chapter: Step 2 – Close the Waiting Room.
I hope you get a chance to discuss these ideas with your colleagues. If you have comments, comments and suggestions, leave them below or email me, so we can discuss them in the next blog / podcast. Thank you!
photo credit: Blue Microphones Yeti USB Microphone, Blackout on Amazon.ca