 Will fee cuts do anything to doctors? Certainly, fee cuts hurt patient care and new graduates. But will legislated fee cuts make any difference to established family doctors?
Will fee cuts do anything to doctors? Certainly, fee cuts hurt patient care and new graduates. But will legislated fee cuts make any difference to established family doctors?
A few mid-career physicians say they don’t expect any real pain from cuts. Others doctors just carry on in over-worked ignorance of anything political. But some physicians are extremely concerned. We might think of these doctors as marginal customers.
Marginal customers are shoppers who hover in indecision before purchasing a product. They are price risk averse. Companies work hard to help marginal customers commit to a purchase. Businesses don’t waste much energy on committed customers who do not, or cannot, change products easily.
A big group of family doctors behaves like committed customers. They stick with office practice and have no easy alternatives. For them, fee cuts demoralize and irritate but will not change what they do for a living.
Another group of family physicians never works in an office. They practise emergency medicine or palliative care or some other medical pursuit. Fee cuts won’t change their careers either.
But many family doctors have a small practice as well as other medical duties. They often work in small or rural communities providing a range of services beyond office care. They balance their ideal of an office practice, where patients are given extra time and attention, and other work such as public health, long-term care, education (unpaid) or whatever else their community needs. But office overhead never sleeps. Even when doctors work outside their office, overhead keeps generating bills. A cut to fees for office work changes financial balance sheets. Non-office work ends up subsidizing office practices, even for docs who work in groups.
Over the last 2 weeks, many readers have shared comments, sent emails, or told me personally how fee cuts impact them. Here’s what they say:
1. Amanda (shared her comments on an earlier blog post)
…I am a family physician in a small town in Ontario and am working other positions (public health, university teaching) to be able to subsidize the cost of keeping my family practice office open. I am definitely one of those docs who is pulling the provincial average down and cannot afford to keep money in the corporation by incorporating or income split as my spouse is a teacher and it would not benefit our tax situation. I adore my job, I love teaching future physicians and believe family medicine is the backbone of our health system. I never thought, however, that I would spend so much time worrying about money after having been in practice 15 years. I have considered closing my practice several times because my overhead runs upwards of 60-70% some months. I can’t cut my expenses anymore and am not willing to sacrifice the quality of my patient encounters to push people through faster.
I know none of this is news to you… I feel validated and among outstanding company in reading your articles and comments. I wouldn’t change my career and feel privileged and blessed to be a small town family doc but believe the government and media are not being accurate in their portrayal of our situation….
…Our small town has lots of unemployment, low education levels and families struggling to put food on the table. I am so thankful and recognize my blessing and privilege in being able to do what I love and be paid anything for it. But – I fear I can’t continue providing this needed service if I can’t keep putting food on my own children’s table….
2. Anonymous Family Doc
One doctor worried that any hint of being forced to reconsider her office practice might cause panic in her community. She has young children and works 40 hours per week. She pursues an idealistic goal of unhurried, holistic care. This keeps her income very low compared with colleagues. Her fixed costs remain. The fee cuts will hit her net income at least 30%.
3. Doctor on Twitter
Dr. M shared that she has 2 young kids and works office based family practice plus ED. She worries whether fee cuts make her office unsustainable.
4. Small Volume, High Needs Doc
Another family doc is approaching the end of his career. He manages more complex/high-needs patients than average. He sees a small number of patients each day but spends more time with each one. His income-to-overhead ratio balances on a razor’s edge. Small changes to gross income produce exponential changes to his net income. Fee cuts force him to seriously consider whether he can keep practicing.
5. Emergency Doctors
A few family docs, who work a number of shifts in the emergency departments, have indicated they will increase their ED work and consider closing their offices altogether. I expect this number to increase.
6. Near Retirement
Primary care reform re-invigorated family practice for many older doctors. They could finally step off the fee for service treadmill. Adding 10 years to the end of their career has helped reduce the number of patients without a doctor from 3 million down to 900,000. Expect these doctors to revisit their original plans and look again at retirement.
Rebuttal
Many people shrug, so what? Businesses go under all the time. It weeds out the weak and leaves the strong. Besides, most doctors probably fall into the ‘committed customer’ group. They have to keep working no matter what the government decides.
Unlike failing businesses, these ‘marginal customer’ family practices provide an invaluable service to their local communities and offer a great example of what outstanding care might look like in less than ideal conditions. The physicians who attempt to provide an idealistic form of unhurried, holistic medical care often provide role models for the rest of us who scurry around in practices that have grown too large.
People need to understand how fee cuts change healthcare. Physicians will work to minimize the effect, but cuts will harm patient care. Losing small family practices won’t just decrease access to care, it will impoverish the whole character of healthcare in Ontario.
photo credit: theguardian.com
 It seems there’s a bullying epidemic. Sometimes it hits you. You pick up your books, brush off your knees, and smear the tears from your eyes. Do you then:
It seems there’s a bullying epidemic. Sometimes it hits you. You pick up your books, brush off your knees, and smear the tears from your eyes. Do you then: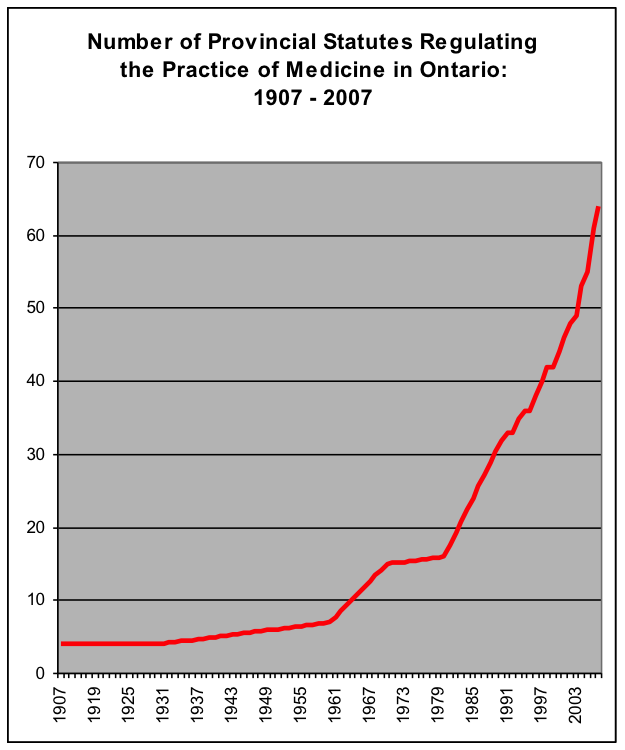 A lawyer friend added up all the statutes that regulate medical practice in Ontario, going back to 1907. Each statute can have many provisions. Statutes spawn even more regulations, but he ignored all these to make a simple point. He graphed his findings on the right.
A lawyer friend added up all the statutes that regulate medical practice in Ontario, going back to 1907. Each statute can have many provisions. Statutes spawn even more regulations, but he ignored all these to make a simple point. He graphed his findings on the right.

