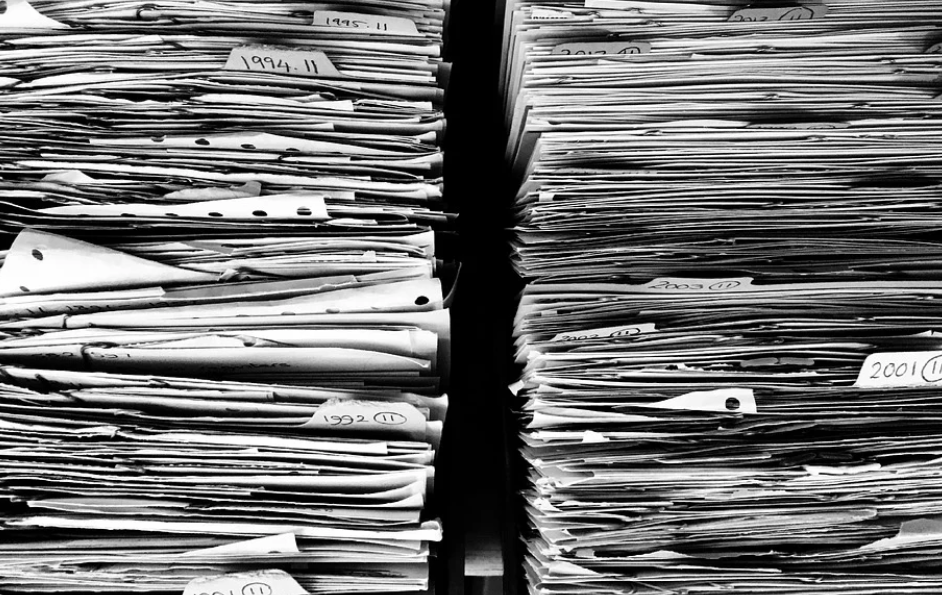
Clinic walls used to sag with special shelves and trays full of forms. Cupboard doors refused to close as forms refused to stay inside. Extra forms always slipped out onto counters and floors, when you tried to yank one out from the bottom of a pile.
A secretary’s job description included being able to answer: “Where’s the form for the new clinic?”
Last time we looked at forms, I aimed at bureaucrats and the heavy loads they tied on doctors’ backs. It was accurate but not entirely fair. Many physicians (most?) love forms and hide an insufferable desire to bureaucratize.
Thousands of Forms
Computers now store all our old paper forms, plus hundreds and hundreds of new ones—over 1,100 in some cases.
One form is for ordering a CT scan at Southlake Hospital. Another for CTs at Markham.
Anything required outside the clinic needs its own form. Hand-written notes will not do.
Inside hospitals, Pre-Printed Orders multiply forms near infinity.
Forms set the standard of practice for all tests, most treatment protocols, and many referrals.
Doctors started designing their own clinical forms for personal use years ago. It started with simple stamps and templates designed to speed the chore of charting negatives—just paste the same idealized note over and over, while adding positives if necessary.
Today, chart-taking excellence means inserting a scoring tool for every clinical question for which a scoring tool exists. The only thing worse than not using a clinical form is not knowing one exists for the clinical problem at hand.
Does your patient feel depressed? There’s a scoring tool for that.
Anxious? One for that too.
Confused? Forgetful? Out of shape? Look in the forms’ list.
Even if you cannot find a form to fit perfectly, you can tweak the patient history a bit. Everyone will think you much smarter for having used a form.
Redundant Forms?
A dozen different versions of a similar form begs for streamlining.
Pray no one takes notice. An enthusiastic manager might convene a committee to help simplify your forms and propel him up the civil service at the same time.
His forms committee will spend six months whittling sixteen, 1-page forms into a single, elegant but thorough 3-page New Form.
The New Form will capture the best of each of the old forms, while reflecting the committee’s vision of an ideal form.
Every detail from the latest literature—no matter how small—will find a spot on the form (in tiny print).
Mandatory fields force users to enter essential system data, which serve no purpose for patients.
Now instead of sixteen simple forms which took only a minute to fill, doctors get to use one that takes twenty.
After congratulating themselves, committee members will take their New Form on tour to collect congratulations from other committees.
They will draft a memo:
–Notice of New Form –
As of such-and-such a date, please use the New Form.
Discard all old forms.
If used, old forms will be rejected and returned.
Responsibility for delay incurred by use of old forms shall rest with the user.
Risk-Free Forms
The quest for better forms raises a bigger point.
Consider the Ontario Perinatal Record (OPR): a five-page form, number 5046-64 available at the Central Forms Repository of the Ministry of Health and Long-Term Care.
A multilateral committee of expert stakeholders created the OPR, currently on version 5. The OPR replaced the Antenatal Record 1 and 2, which was already a long form itself.
The OPR makes management of pregnancy as close to paint by numbers as possible. It includes several hundred data fields, including 53 Yes-No questions with checkboxes after each. There is a spot for everything ever mentioned as having anything to do with pregnancy.
Forms vs Thinking
Herein lie the horns of our medical dilemma.
We want safety. No sane doctor covets risk. To maintain risk, when it could otherwise be eliminated, is mental not medical.
Each form helps. No one remembers all the science. The Ontario Perinatal Record is the apotheosis of evidence-based clinical care. Moms are better for it.
Given the benefit of decreasing risk, doctors welcome tools that promise it.
Why rely on thought when a form can deliver better care without the pain of having to think?
Safety in Forms
Charts filled with forms not only define quality they create a legal umbrella. They turn clinical prose – notorious fodder for lawsuits – into starched, pre-approved, lawyer-proof verbiage. Why give lawyers anything to critique?
What are you suggesting, Mr. Lawyer? Which of my tic boxes do you dispute? Are you disagreeing with the writers of the forms?
Free-form notes filled with patient details are risky. Standardized forms are safe. Ensconced in a bubble wrap of forms, doctors lose touch with the messiness of clinical medicine beyond forms.
Medicine has Changed
Clinical medicine is now like playing darts. Aim the pointer at each box as quickly as possible.
In primary care, forms decrease risk and increase evidence-based treatment. The greatest challenges left are form-less problems: social issues, difficult personalities, office management, and so on.
In all this, we say doctors are burned out. But is this the right word?
Photo credit: Myrfa on Pixabay

Medicine is increasingly becoming a profession where one diagnoses and treats by numbers…the important thing is to know which forms should be used for scoring and which App one should utilize.
Examiners and assessors ( and courts) will judge by which forms or App the particular doctor chose to utilize to reach a diagnosis and which forms and Apps were utilized to determine treatment…with virtual care, patients will be referred to the site, app, form and simply report back the scores…depending on the scores, the app score generated medication will follow.
Virtual CME’s increasingly refer attendees to favoured sites on the internet and apps, to high tech phobes such as myself who uses a flip phone not attached to the internet it poses a problem.
Before COVID, when we still actual human to human CMEs , colleagues would use their iPhones to take pictures of the screen which flashed the recommended sites and Apps, annoyingly obscuring my view of the screen, the recommended sites and apps meaningless.
Eventually I purchased myself an I phone as COVID struck, more because the restaurant I frequented used one of those square jigsaw thingamajigs instead of a menu , I had to point the iPhone at it , photograph it and , hey presto, there was the menu….its medical utilization remains a mystery.
One cannot have a conversation with the youngsters without them turning to their smart phones to fact check or to go through the differential diagnosis etc., their thumbs in a blur…my right index staggers from key to key.
Where forms are concerned, they are changed without warning, rejected because of some unchecked irrelevant box , with referrals delayed….one suspects that they are designed by a malicious Machiavellian bureaucrat deliberately to delay and deflect.
Love your comments, Andris.
I love gadgets and tech. But I bristle at tech telling users how to behave. I guess it’s an old-fashioned belief that the craftsman is supposed to control the tool, not the reverse.
Too many excellent thoughts to respond to them all … I know readers love them … they tell me often!
Thanks again, Andris!
Cheers
Having had my Pfizer COVID vaccine #2 on Wednesday the 16th I wrote my piece feeling exhausted and grumpy..that second dose can take it out of you…night sweats last night.
I feel sad for our profession, Family/ General practice in particular sensing that we are beginning to become expendable middle men in the health care system that is growing into place ( I don’t think that the word “evolving” is correct, the opposite in fact).
The ivory towered CFPC is becoming more and more irrelevant , my grumpyness was compounded by Sohail Gandhi’s excellent response to the CFPC article “ Family medicine is not a business”…” Tone deaf CFPC fails members, embarrasses itself”.
In 1968 I arrived in London , Ontario in the company of McWhinney, one of the fathers of Family Medicine in Canada…he must be turning in his grave at the degeneration of his dream at the hands of the Lilliputians that followed him.
Happy Father’s Day this weekend…or is it Happy Birthing person assistant day?
Night sweats — not good! I hope you are all back to normal now.
I think we have witnessed the proletarianization of the medical profession — especially in family practice. The whole ethos has changed. Docs tell of the late 1980s and early 1990s — only shortly before I started — when they would get an OB to teach them how to use forceps. Having seen one, they would do one with supervision. Then they included it as part of their practice, in the same way they did during residency. The regulatory colleges do not allow that now. You need a six month course (or longer) with an application for a change in scope of practice. As fees dwindle, doctors have to do more non-medical things themselves. We do not diagnose and treat; we educate and motivate. Beautiful clinical notes filled with forms and checklists now define good medicine.
I’d better stop complaining … sorry!
Thanks again for posting.
Cheers