 Imagine that all bakers were nationalized under the Canada Food Act, also known as Foodiecare.
Imagine that all bakers were nationalized under the Canada Food Act, also known as Foodiecare.
Selling bread is too important to leave to bakers.
Bakers may sell bread, but only under special rules, unknown to most customers. Customers need protection. They might buy bread they do not need.
If Sally wants bread, Bob the baker must sell only bread. If Sally wants bread and bagels, Bob must give the bagels for free or ask Sally to buy the bagels tomorrow.
Sometimes, Bob feels guilty and gives the bagels for free. Bob tells himself that he has spare time; the bagels might not sell anyways. Bob often forgets about his mal-baking insurance, continuing baking education, and saving for retirement at 73.
Canadian Bakers for Foodiecare say the cost of bagels is already priced into the average loaf of bread.
Furthermore, bakers have a privileged status under Foodiecare. People always want bread. And Canadian bakers do not have to pay for advertising and administration.
Not Eligible for Payment
In Ontario, it is illegal to bill a patient for medically necessary care if the government has decided that the care in question is “not eligible for payment”.
A patient usually presents with problems that fall in one fee code; he wants bread, and nothing else.
But oftentimes a patient wants 10 loaves, or he wants bread, bagels, and a muffin for his mother-in-law.
The farther we get from doctors and patients working out what patients need in the clinic, the farther we get from Medicare meeting patient needs. Click To TweetNot eligible for payment applies to separate services, both of which are medically necessary.
For example, a patient may present for a Major Eye Exam (A115). At the end of the visit, the patient might say that they had chest pain this morning. The physician must address the chest pain, but cannot bill the government, or the patient, for the care.
The assessment of the chest pain is not eligible for payment.
Medically Necessary
All services in the OHIP Schedule of Benefits (SOB) are medically necessary. Government insurance ‘covers’ all medically necessary services:
“Insured services under the Act are limited to those which are listed in this Schedule, medically necessary, are not otherwise excluded by legislation or regulation, and are rendered personally by physicians…”
But government assigns some medically necessary services as not eligible for payment. The OHIP Schedule of Benefits defines ‘not eligible for payment’ on page GP3:
“not eligible for payment – when a service or a claim submitted for a service is described as ‘not eligible for payment’, the service remains an insured service for which the amount payable is zero
[Commentary: Patients cannot be charged for services described as ‘not eligible for payment’ as they remain insured services.]”
‘Not eligible for payment’ often makes sense. It prevents surgeons from billing a pre-op assessment minutes before surgery and closes other loopholes too.
Furthermore, there are rules about exceptions to rules about not eligible for payment:
“only eligible for payment – when a service is described as ‘only eligible for payment’ when certain conditions are met and those conditions are not met, the service becomes not eligible for payment.
[Commentary: Patients cannot be charged for services described as ‘only eligible for payment’ as they remain insured services.]”
Regardless of what a patient needs, government does not want to pay for the same work twice. That makes sense. However, patients often need more care. If a patient in the emergency department needs more reassessments than allowed, or a bedside ultrasound beyond the 5 allowable US diagnoses, docs must do it for free.
Every case of ‘not eligible for payment’ has a list of reasons to support non-payment. Regarding reassessments and ultrasounds:
They would incentivize useless care
They would incentivize useless U/S scans
A consultant should provide that service
They would drive up costs
They would distort relativity
Remuneration is captured in the general assessment fee
It averages out in the end with simple and complex patients
Besides, docs will do what patients need regardless of fees
So What?
Notwithstanding the good reasons to avoid paying doctors for doing nothing, we cannot forget that fees matter.
Fees drive patient care. It’s why we have fees in the first place (or capitation rates, shadow billing, productivity incentives, etc.). Without a fee to care for problem X, doctors will care for the urgent needs of problem Y.
Declaring medically necessary care not eligible for payment means patients will get less of that medically necessary care.
Even the most altruistic, fiscally blind physician divides her time between equally sick patients. If problem X has no fee and a doctor spends all her time on X, she will soon be out of work. None of her patients will get care.
Fees shape service. If problem X is not eligible for payment on the same day as problem Y, then a doctor must either bear the cost herself of addressing problem X on the same day or book a time for problem X on another day (if possible).
Doctors tell patients why they cannot address problem X and Y on the same day:
It would require a special room; we need equipment; I don’t have time.
These are all legitimate. Even capitated physicians sometimes ask patients to return. But these reasons often rationalize behaviours docs are forced to take because of the billing system.
Instead of aligning physicians’ and patients’ interests to address all the problems together at one time, not eligible for payment rewards inefficiency, especially for patients.
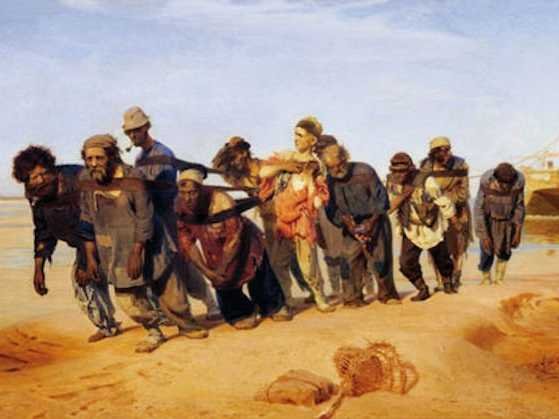
Not eligible for payment makes doctors serfs. In the middle ages, serfs, barons, knights, lords, and ladies all kept feudalism afloat. Serfs rented or owned property in an area controlled by nobles.
Serfs paid the nobles with labour in return for protection and a place in society. At least serfs weren’t slaves.
Delist
If government cannot pay for a medically necessary service, then government should delist the service. We should not pretend that patients will get exactly the same care when a service is not eligible for payment.
Billing rules impact patient care in profound and, for the most part, invisible ways. I wonder whether patients would design a system like this?
“These reasons often rationalize behaviours docs are forced to take because of the billing system.”
The law of unintended consequences.
Exactly!
Diagnostic hearing tests (DHTs) that are “rendered” by ENTs and billed to OHIP should be delisted from the Ministry of Health and Long-Term Care Schedule of Benefits for Physician Services because DHTs are provided for “free” by many hearing clinics. Savings should then be re-allocated to family physicians. Query whether there are other diagnostic tests that should be delisted.
I have no idea if the test is being overused and billed inappropriately but it seems there is a conflict of interest when the one who performs the test “for free” makes money by selling hearing aids. I suspect that the DHT helps the hearing clinics decide which hearing aid is best for the patient.
Having said that, I altruistically suggest that the savings for this and other tests be re-allocated to retired ophthalmologists.
Interesting thread of comments, Perry and Gerry.
I started residency in ENT. I cannot imagine trying to deal with an complaint about hearing loss — covered by OHIP — without being able to perform a hearing test — also covered by OHIP. As to whether we should delist the test, I think that is a worthy debate, as is the question of whether the tests are being done more often than patient need or desire would indicate.
Thanks for brining up the issue. Given the wide variability of a number of diagnostic tests across the province, it seems there might be room to figure out whether huge numbers of patients are not getting the tests they need or whether huge numbers of patients got the tests they did not need.
Either way, medically necessary care that is not eligible for payment is heinous. It is servitude.
Thank you both for reading and posting comments!
Cheers
There is no conflict of interest when a hearing clinic “performs the test for free” and “makes money by selling hearing aids.” because hearing clinics are unregulated in Ontario.
Huh? so the one suggesting that mom needs a hearing aid based on the test performed by the one suggesting mom needs a hearing aid is not really a conflict of interest – notwithstanding CBC Marketplace did a piece showing the average hearing aid is $25 worth of electronics….
Most clinics in Ontario are unregulated including hearing clinics. No laws apply to unregulated clinics.
What if ENT did hearing tests then advised patients to order hearing aids online on Amazon? There was a study presented at a Geriatric journal club stating that they work too. Many patients even after spending 1000s refuse to wear them. How bad could the Amazon.ca ones be for $40-80?
Brilliant suggestion. Thanks Carol!
A patient or a former patient can file a complaint against an ENT with the CPSO. A customer or a former customer cannot file a complaint against a hearing clinic because hearing clinics are unregulated in Ontario. If a hearing clinic is owned and operated by a hearing instrument practitioner, a customer or a former customer cannot file a complaint against the hearing instrument practitioner because hearing instrument practitioners are unregulated in Ontario.
That line about insured but not payable is the first deletion I would put in a new Schedule of Benefits. This language is nonsense and illegal as no one can be legally compelled to work for free. I would also go through quite a few small procedures currently listed as insured but have non-sense fees. They should be de-listed or priced appropriately.
The Ontario Government passed a law in or just before 1990 providing that a service rendered by a physician can be an OHIP insured service without any amount payable by OHIP to the physician for the service. The law has been in place for almost 30 years. There have been no legal proceedings.
Thanks Perry! I didn’t know about that law. I must look it up. And thanks for making the point, Ernest.
It drives me nuts that there are fees for a few dollars: phlebotomy, ECG, urine dip, etc. NOTHING would be less than $20 in any other professional’s office. The fees are so far off from compensating for the labour, equipment, upkeep, etc that most docs do not bother doing them. This creates waste for patients as they have to travel to a lab to get the tests. Total cost to the economy is exponentially higher.
Thanks again for posting comments!
The Ontario Government wants patients to “have to travel to a lab to get the tests.” because labs have a provincial/hard cap whereas physicians do not have a provincial/hard cap. The more tests that a lab does the less that the lab gets paid for each test that it does. There are only 7 labs in Ontario. They compete against each other for a greater share of the provincial/hard cap.
It was somewhere around that time that I recall some items being changed to zero for ophthalmology. One was retrobulbar injection for cataract surgery. An anesthestist could charge but not an ophthalmologist.
The one that really annoyed me was that rather than taking it right out of the fee schedule, the fee for an assistant at cataract surgery was set to zero. Many of us had been working together for years and assisting each other. I believe the fee was specifically changed to ZERO so that we could not bill the patients directly.
As long as physicians continue to provide unpaid services,and cannabalize each other for the same pool of reducing public funds,they will continue to either burnout or find other sources of income.
All docs are smart,but some are pragmatic(find a way),and some have a feeling of moral superiority(and burnout).
Time to switch the channel and demand a parallel private system like the rest of the world (except Cuba and North Korea).
Well said, Ramunas. I like the way you connected moral superiority with burnout. That’s worth exploring in a longer piece… not sure I agree with you on it, but it sure makes me think.
I agree entirely with your ‘pragmatic’ comment!
Thanks again for taking time to read and post a comment!
Shawn always love your thought provoking articles.
If I take a system thinking approach to this problem, it’s ultimately the fee for service model is outdated and its not meeting the needs for both physicians and patients. This discussion of what to list and enlist should eventually become less relevant if we make payment models more aligned with value and outcomes. We also know that 70% of new mDs don’t wish to work in FFS models and want better work life balance.
I am curious why havent alternative payment models for primary care not spreading fast enough ? Also, I wonder with the burnout epidemic is it the right time where physicians can push for payment reforms and garner public support especially for primary care.
Also, is copayment a viable and likely option to help offset these economics woes?
Great comments, Ali
I agree. Fee for service (FFS) makes the problem most obvious. Having said that, everyone’s pay determines how they behave. It does not matter whether docs are on straight salary, APP with shadow billing, or salary with productivity incentives. Different pay structures create different behaviours. If it did not, then we could just pay docs a lump sum at the beginning of the year and ask them kindly to see patients. What do you think would happen? 🙂 The hard work is to figure out what kinds of payment mechanisms best align patient needs with MD interests….or in other words, which approach best aligns patient and MD interests.
Co-payment is a big and different (although related) question. I have never blogged on it. Perhaps I should. I won’t share my thoughts on it here. Some readers might not know that Tommy Douglas was a firm believer in co-pays…at least at the start. He might have recanted later in life.
Thanks so much for taking time to read and post a comment!
Cheers
The combination of the complexity of the SOB, codes that are payable at nil, low fees for the services delivered and not getting paid for the work that is done (one assessment code per visit not per issue dealt with) speaks simply of the contempt that the MOH/government has developed, stoked and honed over the past 35 years.
We are loathed. Making us do things for free provides some sort of perverse satisfaction for those with blinkers on who see us as a line item and fixate on fiscal annual gross billings. It is human nature to hate those that make more than you. How hard they worked and sacrificed to get there…how many patients they cared for and services they provided…is all immaterial. It is all about that end of year number…and doing whatever can be done to keep it down.
It is all laid at the feet of our profession. We have to pay for being free, being in demand and being busy. We have to subsidize the medical care of the populace with our low fees and we are expected to be the poster child for ‘sustainability’ by continually working harder for less. Oh…and we’re expected to forego increases and take more cuts to help the province deal with the debt. No other profession paid solely by government has to do this because…well they have rights and unions, you see.
The perfect storm is here…and now. Students with hundreds of K of debt increasingly cannot match to residencies. Those lucky enough to become residents are increasingly having to become ‘permanent’ residents through fellowships because there are no jobs for their services (or they leave). Running offices with increasing overhead in the face of mounting cuts is becoming so onerous that increasing numbers of practicing physicians are looking for any possible exit. And the government and the public want more and more for less and less. For the profession, this is no longer sustainable. The time to fix this is now or this ship is sinking forever…