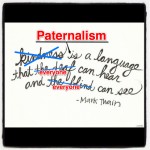
Medicare assumes fixing patient problems is crucial, and being nice, less so. We prefer polite, but don’t believe it’s essential.
Medicare assumes fixing patient problems is crucial, and being nice, less so. We prefer polite, but don’t believe it’s essential.
Jill Dean, CEO of Brand Biology, gave a presentation “Grumpy Tech Meets Grumpy Customer. This Can’t End Well … Or Can It” at a recent customer experience conference. (Thank you, Bruce Palmer, for tipping me off to this!)
Check out the 30 min. presentation on YouTube.
Virgin Media sends out technicians to help customers with cable service problems.
Techs arrive at customer’s homes harried and edgy. Customers call when they have problems; when they are frustrated. Like healthcare, both provider and customer are often frustrated long before they meet.
Virgin tried to figure out what drives client satisfaction: technical skill or pleasant service.
They asked customers to score service on a scale from +100 (happy customer who would recommend to others) to -100 (unhappy, no recommendation). They found that when technicians:
Fixed the problem and were friendly and polite, customers scored +74
Fixed the problem and were neutral in tone, customers scored +26
Fixed the problem and were rude, customers scored -44
Did not fix the problem and were friendly and polite, customers scored 0
Did not fix the problem and were neutral in tone, customers scored -64
Did not fix the problem and were rude, customers scored -87
Rudely fixing a problem was worse than being nice but not fixing the problem at all.
No doubt, if “fixing the problem” equals saving life, people prefer having their problem fixed. However, only a tiny percentage of people seek care for life-threatening problems. Canadian emergency departments send 89% of patients home without life-threatening diagnoses.
We need to align system incentives so that everyone works to provide great customer service, not just fix problems. We should aim for every patient to recommend us to their friends.