I convinced myself I was dying of prostate cancer last year. Turns out, I was drinking too much coffee.
Patients often seek help for things that turn out to be pretty simple.
They laugh afterwards.
Phew!
Thank God it wasn’t cancer.
Many physicians sincerely believe that their staff can safely dismiss a patient’s concern over the phone, or put off seeing a patient for days (or weeks!).
By the time someone has ramped up the courage to seek help, his anxiety has peeked; he can’t take it any longer.
Patients finally give in and get seen; like Lightning McQueen finally going to buy some tires in Cars:
Lightning McQueen: All right, Luigi, give me the best set of black walls you’ve got.
Luigi: No, no, no! You don’t know what you want! Luigi know what you want!
Avoiding Patients
When patients want to be seen in the office that day, physicians argue that:
- They know it’s not a serious problem.
- They know it can wait.
- They know the patient will be fine.
- They know best.
Patients often think they need medical help when there’s nothing medically serious going on.
But, unless physicians get radically committed to understanding and meeting the perceived needs of patients, medicine will lose the privilege of caring for patients’ concerns or be tolerated begrudgingly until some better option comes along.
How soon would you like to see your family doctor if you called for something that really worried you? Do you like getting a “We know best” attitude? Do you like having to worry while you wait for an appointment?

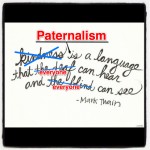
Some people who call for an appointment are the way you’ve described. Others are not. In a Family Practice, people may indeed call because they are worried something serious is going on, but it is at least as likely that they have a symptom they have been seen for by multiple providers on multiple occasions, or that they have paperwork for an entitlement. The great thing about Family Practice, as opposed to an Emergency or Walk-in, is that an experienced and perceptive receptionist can often sort this out, fast-tracking the group you have identified, while keeping the others under control (paternalism?). Physicians can lay out some principles for this, but depend on their (often under-appreciated) receptionists to make it work. -philw-
Great comment!!
No one can argue that some patients do worse when we support bad behaviour. In the ED, I think of well know narcotics seekers who scream and yell, writhing in pain creating a bigger scene than every other patient in the building. Running to attend will only encourage the behaviour next time.
I worry when staff (nurses, triage, clerks, receptionists) put patients off, with full support from the MD in charge, for what they believe to be insignificant medical concerns. I don’t mean the few patients who call everyday, or the ones with more disability forms that need to be filled out NOW. I refer to the bulk of patients who rarely have an urgent concern for whom physicians argue it’s perfectly okay to defer because, “It doesn’t sound like it needs to be seen right away.” Putting provider needs over patient needs runs deep in healthcare; it shows up when you start to push providers to change.
One last comment I didn’t add in the post, it makes no sense to expect community providers to see patients promptly without giving them the support to do so. Why would you work up a patient with chest pain in your office if you don’t have access to stat/acute lab, ECG and DI services?
Thanks again! Have a great weekend.
Shawn