Minister Hoskins said that doctors got a 61% raise from his government. On top of that, he gave doctors a $142 million increase in their earnings this spring. And people believe him (see Duelling Doctors and Ontario Imposes Cuts).
Minister Hoskins said that doctors got a 61% raise from his government. On top of that, he gave doctors a $142 million increase in their earnings this spring. And people believe him (see Duelling Doctors and Ontario Imposes Cuts).
People believe a big lie much easier than a small one. Small lies get compared with reality; people spot them quickly. Big lies stand alone in space; there’s nothing to compare them to. (see “The Big Lie”)
Who wouldn’t love a 61% raise? When is a $142 million wage increase not a good thing? Voters must think that doctors, supposedly smart people, are quite stupid, greedy, or both.
Wage Increase
Let’s look at the alleged $142 million wage increase first. It means that the Minister of Health would give every doctor in Ontario $5260 ($142 million / 27,000 doctors).
Most people see through this. The population grows by 140,000 per year. An aging population requires more services, and we graduate 700 new MDs every spring. For these reasons, and many more, healthcare services grow in Ontario by $350 million annually. Growth in physician services is called the utilization rate and runs about 2.7% each year (sometimes much higher).
In reality, Hoskins’ offer to increase spending by $140 million turns out to be a promise to underfund growth by around $200 million. His wage increase is actually a claw back from every physician in the province.
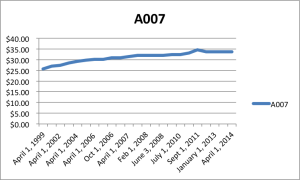
Doctors Raise – 61%
My friends and family have never heard of a 61% raise. They wonder how it could be true. Did doctors actually get a 61% raise?
The Canadian Institute for Health Information (CIHI) serves as the gold standard for healthcare data in our country. CIHI shows that provincial spending on doctors was $4.510 billion in 1995. In 2013, it blossomed to $13.185 billion.
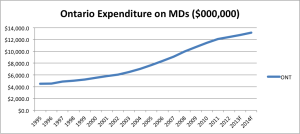 Focusing on the part that Hoskins takes credit for, the province spent $7,024.8 billion on doctors in 2004. In 2014, it spent $13,184.8 billion.
Focusing on the part that Hoskins takes credit for, the province spent $7,024.8 billion on doctors in 2004. In 2014, it spent $13,184.8 billion.
Reporting the Change
There are at least two ways to look at spending.
1) What it means to governments.
If you were paying the bills, you would want to know, “By what % have we increased spending on doctors over the years?” Finance departments care most about changes in total spending.
Using CIHI data, this approach gives an increase of 88% spending on physician services between 2004-2014. If you calculate the change since 1995, the province spent $8.675 billion more, a 192% increase ($8.675/4.510*100%). There’s no question that provincial spending on doctors – on all of healthcare – is growing fast.
2) What it means to individuals.
If you were a physician, you would want to know what the spending change meant to you personally. Does this mean you have 88% more cash in your pocket in 2014 compared with 2004? Did you get a gigantic raise?
This really irritates doctors. No one reports their income going up the way politicians report provincial spending. People talk about annual rates of return. People want to know how much of an increase you got on your income year over year.
If we assume there were the same number of doctors in 2004, doing exactly the same work, caring for exactly the same number of patients, then doctors got a 6.5% raise each year between 2004-2014. But everyone knows that’s not true.
Since 2003, there are 4000 more physicians and 1.4 million more patients in Ontario. On top of that, baby boomers just entered their 60s in the 2000s and there are far more visits required for screening, testing and monitoring than even 15 years ago. As we saw earlier, utilization drives up spending by at least 2.7% per year.
But even if we account for utilization, doctors appear to still get a 3.8% annual raise between 2004-2014 (6.5% – 2.7%). That seems high. Even after inflation, it means doctors got a 2.12% annual raise between 2004-2014 (1.68% inflation for same period). That equals a 23% total increase over 10 years after inflation. We can compare this to other increases in the public sector in another post (they are similar by the way).
Just because doctors didn’t get as big a raise as Hoskins says, doesn’t mean doctors deserved even as much as they got. Does Hoskins still have a point?
History: Raises vs. Cuts
The OHIP schedule of benefits used by the government to pay doctors – the reference book of fees that doctors bill – started out as a copy of the Ontario Medical Association’s own schedule of fees in 1978 with one vital difference that we’ll get to in a moment. The OMA created its own fee book in 1922, long before Medicare, to give doctors some sense of what physicians should bill for services across the province.
The critical difference between the government’s fee book and the OMA’s was that the OHIP schedule paid only 90% of the OMA fees. When the government adopted the schedule, doctors agreed to get paid at only 90% because government promised to pay 100% of bills. Whereas some bills were never paid in the olden days, OHIP pays all the time, if patients have a valid health card.
You can guess what happened over 4 decades. Each year, the OMA used inflation as a guide to adjust the OMA schedule of fees. The OMA did not give itself a raise. At the same time, every 4 years or so, the government negotiated or imposed sub-inflationary contracts starting in the 1970s. Today, even after all the generous increases from the Liberal government, the OHIP schedule of benefits pays only 50% of the OMA schedule of fees.
Bottom Line
Doctors did get a raise over the last 10 years but nothing compared to the 40% decline in fees since 1978. After decades of sub-inflationary increases, the government realized that family medicine had been decimated; students avoided it. The government started to invest some of the federal health transfers to rebuild family practice, the cornerstone of all great healthcare systems.
The irony about Hoskins’ 61% is that he can’t have it both ways. Either it’s proof of great work by his government in 2004, 2008 and 2012, or it’s another scandal like eHealth, ORNGE, and the gas plants. Either it was a solid rational decision to negotiate the raises in 3 separate contracts, or it was another bad decision to add to the pile.
Painting this mess as doctors’ greed is just obfuscation. In the end, very few people will read and consider a post like this. Politicians know that. They know that throwing out a big number will stick in voters’ minds better than a complicated explanation of why the number is wrong. We need to make these fee cuts about patients’ access to care and healthcare experience. It’s still what matters most. What do you think?
References:
CIHI report Physician health cost drivers
CIHI slide show (very cool!) on spending across the country
Historic Canadian Inflation rates.
Discount Rate Calculator from MoneyChimp
Bank of Canada Inflation Rate Calculator Very fun to play with, too!
photo credit: Twitter.com