 “But your patients expect to see you,” she said. “It doesn’t matter if it’s 8 o-clock at night… When I need my doctor, I expect him to answer.”
“But your patients expect to see you,” she said. “It doesn’t matter if it’s 8 o-clock at night… When I need my doctor, I expect him to answer.”
My mother’s words still echo 25 years later. She nursed 2 floors of Alzheimer’s patients by herself. She’s practical and tough with medical concerns. She managed most things without any support, largely alone, at night, with very sick patients.
When she finally calls a doc, she expects an answer.
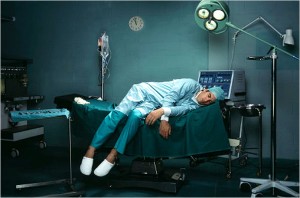
Physicians used to be available 24-7. They slept in hospitals as much as home. It grew out of guilt, duty, greed, social expectations, escape from personal relationships…a complicated list.
24-7 created some odd physicians.
People now realize that healthy providers give better care. Patients benefit with doctors fully engaged, fully aware.
Guilt
“There’s a patient who needs…[some great need]…up near [some place 40 minutes away].”
The one, lost sheep…
Often lost sheep have many people who could help and might even do a better job of helping. But physicians feel a ‘proper’ doctor would go and attend.
Driving 30-40 minutes, one way, to see one healthy patient while making 8-10 other patients wait or rebook appointments is not model behavior. It is not altruistic. It is profligate, wasteful.
Healthcare Waste
Payers and auditors obsess over unnecessary tests and visits. They care less about efficient use of physician time.
Patients benefit when physicians spend time with them.
No matter what else planners dream up, the system should always maximize physician efficiency to keep maximum time available for patients. Regulations, bureaucracy, forms, record keeping for 3rd parties, audits, and quality improvement projects must be measured by the time they steal from patients with their doctors.
Guilt & Waste
Provider guilt works like another layer of wasteful bureaucracy. It often makes physicians steal time from dozens of patients by pretending to model sacrificial behavior for one. Guilt often blends with pride; providers like people to know about our sacrifice and hardships. Often our stories of sacrifice are examples of time stolen from other patients who needed us more.
Efficiency is…
Everything we do means something else cannot be done. Thankfully, patients now expect their physicians to maintain their personal and family life.
We need the system – and all the providers in it – to insist physicians stay maximally efficient. Before all else, healthcare efficiency should start with measuring how much time physicians could be spending with patients if they didn’t waste it somewhere else.
Photo credit: nytimes.com