The Hub published my op ed. You can read it at TheHub.ca or below. Enjoy!
When it comes to fixing health care, governance matters more than policy
Without good governance, new policy will struggle with implementation like all the old policy.
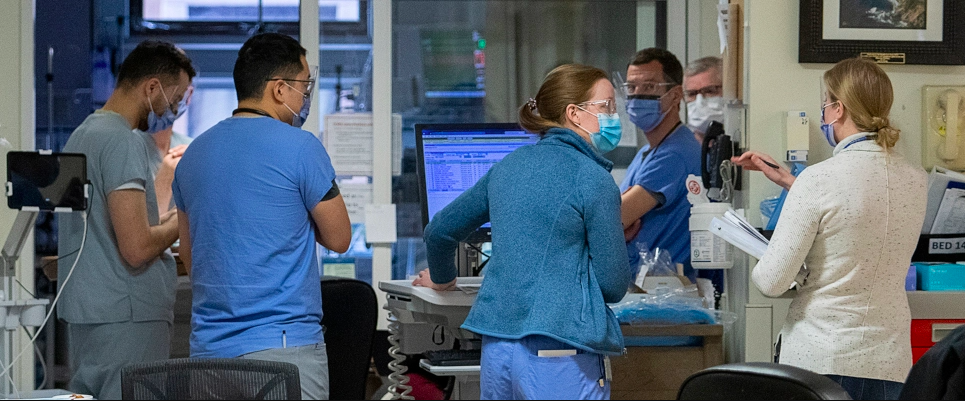
Few voters had first-hand experience with hallway medicine or Canada’s world-famous wait times before the pandemic. Lockdowns changed everything. Health policy failure moved from fear-filled headlines into a tangible crisis everyone could feel.
Failure begs for better policy, or new policy to fill gaps. Planners and policy writers jump to offer solutions: surgicenters, funding reallocation, redesigned models of care, and so on.
New policy, however, cannot fix old policy, unless we know why the old failed in the first place. Most policy fails on implementation, not from bad design. Furthermore, we cannot fill policy gaps unless we understand why gaps exist. Gaps form around constraints and incentives, not from a lack of creativity. The policy environment dictates viable policy options.
How a system functions has more to do with how its governed than with the policy ideas in play. Implementation failure, constraints, and incentives all fall under the larger umbrella of governance. Governance and policy overlap, but they are different.
To fix health care, we need to start with governance: how do we make decisions? Who gets to make them? If we do not, a new policy will deliver the same old results.
Policy to the rescue
Take surgicenters as an example. Surgeons and specialists join together to build a non-hospital, outpatient surgical facility. Each centre offers a specific basket of specialty care, for example eye, orthopedic, or endoscopy services. Surgicenters can offer comfort, convenience, quality, and efficiency that hospitals struggle to match.
Surgicenters exist around the world. They are not new. In Canada, we have been trying to move care out of hospitals for decades. We want to save money and shorten waitlists. Why aren’t Canadian cities littered with surgicenters?
Current incentives and constraints make surgicenters impractical and onerous. Currently, hospitals supply nursing care, equipment, and use of the facility. Physicians use everything but do not pay for it, making non-hospital facilities a tough sell. On top of this, billing rules, regulation of independent health facilities, licensing for necessary lab and imaging services, as well a basket of other restrictions all weave together into a policy environment intolerant of (publicly funded) independent facilities.
We do not need a policy about surgicenters. We need research on why surgicenters do not exist in the first place and what to do about it.
Thomas Sowell, American economist and author, said once, “The most important decision about every decision is who gets to make the decision.”
Sowell expanded this in his book, Knowledge and Decisions: “The most fundamental question is not what decision to make but who is to make it—through what processes and under what incentives and constraints, and with what feedback mechanisms to correct the decision if it proves to be wrong.”1
Before making a change, every hospital administrator must ask, “Who needs to be in the room?” Spectacular new policy will fail in even more spectacular fashion if you ignore governance. Informal governance can matter even more. Decision makers are often not the ones listed on the organizational chart: colleagues influence through personality without title or position.
Governance eats policy for breakfast
Peter Drucker, the legendary management consultant, once said, “Culture eats strategy for breakfast.”2 We can say the same about health policy: governance eats policy for breakfast.
Dr. Dave Williams, a former astronaut and leader at NASA, served as CEO at Southlake Regional in Newmarket. He said, “It’s not clear who runs the hospital.” He was making an observation, not a complaint. “Compared to what I’m used to, it’s challenging to get things done.”
Without clarity and fidelity to best practices, governance will drift. Sowell, again, sums this up:
Even within democratic nations, the locus of decision making has drifted away from the individual, the family, and voluntary associations of various sorts, and toward government. And within government, it has moved away from elected officials subject to voter feedback, and toward more insulated governmental institutions, such as bureaucracies and the appointed judiciary.
Is this a problem in Canada? Brian Lee Crowley, managing director of the Macdonald-Laurier Institute, thinks so. Governance drift leads to central design—a temptation for all political parties.
In his book, Gardeners and Designers: Understanding the Great Fault Line in Canadian Politics, Crowley dilates on how gardeners approach governance.3 A gardener prepares the soil, removes waste, provides support, and tends to progress. Gardeners celebrate the surprise inherent in what grows and blooms. They do not manage growth for a specific policy outcome they designed in advance.
Designers dream about how to make health care better. Gardeners ask the more important question: how can we get good ideas to grow? A gardening approach to governance leaves plenty of essential (gardening) work for government. It empowers those closest to the problem and leaves design, experimentation, and implementation to them.
We cannot try to “fix” health care with new policy. Without good governance, new policy will struggle with implementation like all the old policy. We need to do first things first. Governance eats policy for breakfast.

This takes intellectual convolution to another level … lol.
Basic conversations about egalitarianism …. our system is not because if you know someone you go to the front,and if you have money you go to the USA.
Basic conversations about funding … totally public funding is unsustainable and we need to find a way to get private monies involved like European hybrid systems.
I guess both of these speak to governance …. which will change only when the system implodes enough,which may be happening.
I have never seen doctors or patients as unhappy as at present.
Exactly, Ram: “…both of these speak to governance…”
Governance impacts funding decisions also — absolutely. This might be the only governance decision people know about! Whatever happens, we must not let anyone except government have final say about funding.
What people do not (almost never) think about are the millions of decisions required to deliver care. Most doctors don’t think about them either. They assume they just see patients and practice medicine. They do not wonder about why clinical care is shaped the way it is; they just assume it is a given, like air or sunshine.
I don’t mean to be harsh. It’s just that most docs have other things to think about.
Who gets to make the decision is the most important decision. I wish we’d make this more widely known and discussed!
Great to hear from you.
Cheers
Health care in Ontario has been slipping and sliding towards the abyss over the last 50 years.
As a consequence of 50 years of decisions , some wise, many hare brained , made by voters, politicians, bureaucrats, health care “experts” and “ academics” , political “philosophers” here we are faced by a massive fetid Gordian knot.
Many mistakes were denied , lessons were not learned, as a consequence the errors compounded over the decades and here we are…no one is happy , not in the ranks of the medical profession, their patients, the massive health care bureaucracy and the career politicians who reached the levers of power by making unrealistic promises.
As a consequence Canada’s health care ratings on the world stage is slipping, ever slipping….morale in the health care field continues to deteriorate remorselessly with no faith in the various positions of leadership within the profession and outside.
There is only one way to deal with a Gordian knot and there is no Alexander in sight.
Great last line, Andris. Well said.
We have a mountain of mistakes made over five and a half decades with no one to hold to account. On top of that, the current governance dysfunction guarantees more chaos and disorder will follow.
My years on MAC (Medical Advisory Committee — the highest governing medical body in every hospital) can be summed as a group of doctors working to hold administrators to account while trying to ask for resources to provide care and administrators playing their cards close to their chest while trying to say no wherever possible (without being too obvious).
Thanks again for posting!
Cheers
Here’s a reply to an email from a responsible (and responsive) Canadian Provincial Legislature Member.
I trust this elected representative and have heard similar words directly from others, including from the Health Minister personally.
– – – – – – – –
“I know you are tremendously frustrated with this situation, and I appreciate your input. Thank you for your recent email. I do use your insight to raise issues within caucus and having your assessment of the situation helps to encourage us to do what we can.
That being said, the ability of the government to impact 🏥 quickly is hampered by the necessary separation of powers that exist between cabinet and the organization. The legislative branch of government can’t just go in and make personnel tweaks in individual departments.
However, as you point out, there has been a lack of accountability and leadership within (🏥) for some time. As you know, a change is being made in the CEO position within (🏥) perhaps this is long overdue, but it is being made.
Investigations into these matters also are very tricky as they can quickly become a wedge used for politics. I know you would like to see the results of the independent investigation immediately, but it will take time to do it right.
Budget 2022 has also introduced immediate funding for more (🏥) as well as equipment costs. We need more bodies and (🏥) the system and a better plan to utilize the people and equipment we already have.
I am always available and receptive to your feedback and ideas. I appreciate the passion that you have for our (🏥). I hope you know from our interactions that I am also passionate about improving the care our riding and rural areas receive. I will keep pushing for change in every way that is available to me.”
– – – – – – –
The real or perceived ability to act, by those we elect to govern, seems to be inadequate when substantive changes are needed. Does healthcare culture need to go over a cliff to change?
Thanks for sharing this, Don!
What’s fascinating, for me, is that this MPP seems to be saying he/she cannot act MORE to change the system. He/she seems to want to be able to direct policy change, but the department responsible for change is not directly controlled by the legislature.
The whole point is that the medical industry does not need control by the executive branch of government nor the legislative branch.
It’s the same old story — all political parties do it — “Just let us have control. We will show you how it SHOULD be done.”
The legislature and government have so much work they could do besides micromanaging medicare. Instead, they insist on tweaks and fiddling while ignoring their core duties.
Thanks again for sharing this!!
Cheers
I enjoyed reading your article as well as the comments. I have nothing new to add but perhaps a slightly different slant on a few aspects. In every country and society you get better health care because of who you know even Canada all be it it is illegal. In every country I know of you get better health care including Canada if you have a lot of money but in Canada it is again illegal as it is actually a bribe. Any service we receive should be assessed on the bases of upside downside and often one of the determinants is the cost but not in Canada. Of course I am only referring to in hospital care and Physician Services. We have a strange fee for service system where the receiver of the service is not at all responsible for the fee in fact seldom knows the cost. A system ( in this case delivery of health care that doesn’t take human behaviour into the picture and includes misinformation will never work. We as a society still have to make the system available to all no matter their means.
Great points about human behaviour, Graeme. Our system works great in theory but not so in reality. It’s like blaming “market distortions” for every failing of the market. (To be clear, I think free enterprise is the best we’ve got, but I do not think it is omnicompetent.)
Thanks for posting!
Rant on. All received in my inbox in the past month:
A/From Dr. Nancy Whitmore,CPSO
Good morning,
I welcome you to our most recent issue of eDialogue magazine. Our cover story explores how we all become stronger by uniting together. Allyship — Dictionary.com’s 2021 “Word of the Year” — is one of the most important ways we can address health inequities. As physicians, we tend to want to identify problems and fix them. Good allyship requires us to listen and learn. We need to listen and learn from marginalized communities, and be willing to look inward as well. I hope that you’ll take the time to read this article.
We can demonstrate allyship, for example, during the month of June by celebrating the lives of 2SLGBTQIA+ people during Pride Month festivities and committing to dismantling barriers that affect their access to quality health care. As an article in this issue makes very clear — the need for gender-affirming health care is much needed. We interview physicians — true allies — who are committed to building capacity in the system for their trans patients.
B/From the Royal College of Physicians and Surgeons of Canada
• Nominate an inspiring humanitarian. One of Canada’s most prestigious medical awards, the Teasdale-Corti Humanitarian Award is for Canadian physicians who go beyond the accepted norms of routine practice. Deadline date to submit a nomination is September 30, 2022.
• Celebrate a colleague who’s an Indigenous health advocate. Recognize excellence in your colleague devoted to the rights of Indigenous Peoples with a nomination to the Dr. Thomas Dignan Indigenous Health Award. Deadline date to submit a nomination is September 30, 2022.
C/From the CMAJ,
PODCASTS
Suicidality crisis among transgender adolescents
In this episode, Drs. Blair Bigham and Mojola Omole discuss troubling findings in the recent study: Suicidality among sexual minority and transgender adolescents. Joining them are Mila Kingsbury — one of the study authors — and Dr. Tyler Black, medical director of the pediatric psychiatric emergency inpatient unit at British Columbia Children’s Hospital.
And finally from the OMA (who apparently have my back-good to know)
D/ Everyone deserves a good health-care system, including you
Dr. Rose Zacharias, OMA President
I have been OMA president for six weeks and my heart is breaking. Our health-care system is broken and I see a lot of suffering. No one’s geography, gender, socio-economic status or ability to advocate for themselves should determine whether or not they receive good care. As physicians, we should operate inside a system that makes sure of that. But we don’t. Also, this broken system is breaking us and that is really bad. This organization has your back. You are not alone.
Did you know?
• We held a media briefing last week to address the disparity of care among the LGBTQ community. I was joined by a panel of our skilled and compassionate colleagues who are making a difference in this space. I am so proud of them. The OMA is on the right side of this problem and I am grateful for that. Physicians and allies will be marching in the Pride parade this year on June 26. Consider joining us!
Rant off.
I’m an idiot surgeon. So it’s great that Dr. Zacharias and OMA “has my back.” Otherwise, I doubt I could cope. I would actually prefer if Dr. Zacharias didn’t have my back. It worries me.
However, I do speak with my family practice and emergency medicine colleagues, and they too receive these missives and wonder what is going on with our physician leaders. Is this the best that we have to offer?
The government is laughing at us. Our medical organizations are laughing at us. I would as well given the above. The state of logical thought given our current circumstances in trying to treat patients in a timely fashion is deplorable. Yes, culture does eat strategy for breakfast. Strategy, what strategy? Perhaps that’s the point. If you don’t have a strategy, it’s probably best to fake it with distraction-“Squirrel”.
“We have a mountain of mistakes made over five and a half decades with no one to hold to account. On top of that, the current governance dysfunction guarantees more chaos and disorder will follow.”
I have had the fortune (or misfortune) of having entered medicine by way of a Math undergrad. The first thing they teach you in Math is that any trend destined to end will in fact do so. Can you spot the trend in the four examples noted above? The second thing they teach you is that the trend can remain irrational longer than you can remain sane (or solvent). The rest is commentary. Appreciate the blog very much.
Wow. Powerful comments, David.
“The state of logical thought given our current circumstances in trying to treat patients in a timely fashion is deplorable.”
I edited your comments to put that line in bold. Although everything you said was excellent; people wouldn’t believe it if you had not copied and pasted the exact messages we are receiving (brilliant).
But your line about the state of logical thought nails it. We face the greatest health crisis in many decades — literally millions of delayed procedures. Our leaders prefer to speak about a small cohort of suffering patients. We can only assume it best serves their political purpose. Why else would anyone ignore the far greater carnage to demonstrate one’s woke bona fides?
Maybe logical failure puts it too nicely. Regardless, it presents a failure we can fix, so I think it’s an excellent place to focus.
Thanks so much for posting this. The moral high ground (in my mind) remains the issue of patient morbidity and mortality due to care denied by world-famous wait times and rationing of care, technology, and human resources.
And thanks for your kind support!
Virtue signalling is far easier and more lucrative and career promoting than rolling up the sleeves and grappling , getting dirty and bruised, with the very real medical world problems that need real solutions not balm or band aids.