Given enough fear, people welcome control.
Given enough fear, people welcome control.
Sickness and trauma scare us. Patients need to hear, “It’s okay. Don’t worry. You’re going to be all right.”
Fear begs action.
Scared people want someone in control. In the past, doctors and nurses calmed fears. Patients just focused on recovery.
Medicine got better. Worry about sickness decreased, and worry about hospital bills increased. Losing homes became as much a concern as losing health.
Media sells on fear, especially in the USA:
- Medical Bills are the Biggest Cause of US Bankruptcies – Study
- Why Medical Bills are Killing Us (TIME Special Issue)
- Sticker Shock: Investigating the High Cost of Hospital Bills
Desperate Times Call for Drastic Measures
Extremis malis extrema remedia
Pundits leverage people’s dread of sickness. Panic about rare, high-cost medical catastrophes justifies command and control over delivery of everything else.
People don’t panic over high blood pressure or diabetes. But most healthcare dollars go to chronic disease and risky behaviour in the USA and in Canada.
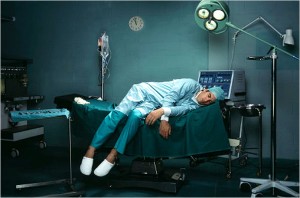
Paradoxically, central planners back off a little in the provision of high profile, newsworthy medical care. Trauma care works best when doctors set up systems guided by outcomes. Bureaucrats let medical experts design delivery and just pay the bill; it’s a much smaller portion of healthcare spending anyways.
But fear about medical bankruptcy justifies more and more micromanagement of everything else.
Healthcare Control
Service, quality and efficiency needs empowered front line providers. Patients suffer when physicians are bound by rigid guidelines, shackled by fear of lawsuits and motivated by perverse incentives. Patients benefit when providers are incentivized to meet patient needs, not system rules.
Command and control does not work in business (Command and Control Leadership Doesn’t Cut it Any More – Globe and Mail). It will never work in healthcare. But fear continues to justify military-style leadership leaving patients on the sidelines as costs.
Most of us support a safety net for rare, catastrophic illness. It’s dishonest to use legitimate fear about medical catastrophe to allow central healthcare control that harms patient access, service and quality. For the bulk of healthcare spending, we should empower patients and providers and let them drive service, quality and efficiency. We should stop supporting central command and control.
What do you think? Do we need more centralized, bureaucratic healthcare control or less?
Photo credit: engageforsuccess.org. Check out their post on Command and Control.