Before medical politics died in Ontario, a PPSA vote meant three hundred doctors from across the province packed into the basement of a hotel in downtown Toronto.
A room full of frowning doctors debating fees was much like kids lighting matches near a haystack.
Inevitably, someone would yell at the board, insult a colleague, or slander the government. Every so often, the Chair would wack away with his gavel, completely ignored by the angry mob.
At one meeting, a red-faced little man stomped several hundred feet across the front of the room and shoved his face in front of another doctor. The angry man had taken offence. He demanded an immediate apology. Or would the other member care to step outside the chamber?
PPSA VotE Needs More Data
The PPSA appears to offer a 1 per cent increase per year with (hopefully) 2.8 per cent in year three.
But what does this mean?
How do specific fee cuts impact income?
Do we have to work 10 per cent harder for a 1 per cent increase?
How does inflation impact the outcome?
How is income impacted by elimination of thresholds and system redesign?
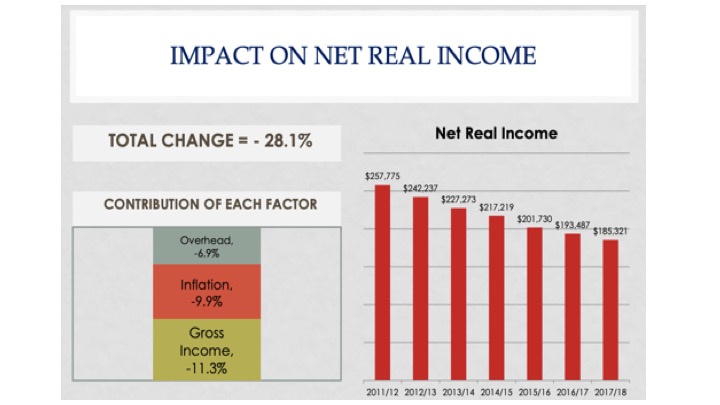
The OMA used to publish fancy graphs of how physician income has changed relative to inflation. The graphs ended when they became too embarrassing.
Governments changed, but OMA performance stayed the same. Endless sub-inflationary increases imposed by successive governments made the OMA look bad.
In 2015, we pushed the OMA to publish an analysis of net income. It showed a steep decline from 2011 to 2015, with an expected 28 per cent cut by 2017-18:
Hazard a Guess At the Cuts Now?
Let’s hope the OMA offers an update. In the meantime, we can try to do our own.
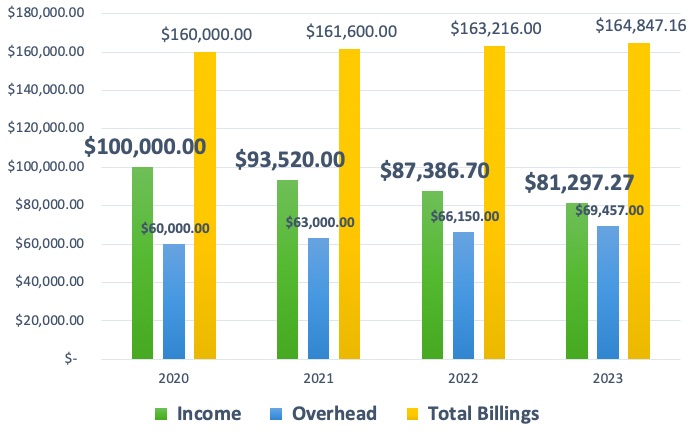
Consider a physician who bills $160,000 and pays $60,000 in overhead (37.5 %). The total billing will increase at 1 per cent for 2021 and 2022, and 2.8 per cent for 2023.
Let’s assume a general inflation rate of 5 per cent. This means office overhead will grow at 5 per cent each year, and spending power (net income) will decrease by 5 per cent each year.
Medical overhead always outpaces inflation, and general inflation may be closer to 7 per cent, but let’s be conservative.
This gives us an 18.7 per cent net decrease over three years. You will feel like you have 20 per cent less to live on. If inflation runs over 5 per cent, a much higher cut seems reasonable.
Add in all the other specific cuts as they apply to your own specialty.
A Fair Process?
Failure to ratify used to mean rolling the dice at arbitration, but at least you got a second chance.
But the chair of the board of arbitration has warned doctors. Do not expect fee increases; arbitration is already fixed.
This makes arbitration a sham.
The whole point of arbitration was to avoid predetermined outcomes. Remove the power imbalance. Enforce fair bargaining. Do not let one side (government) predetermine the price before negotiation even begins.
But Premier Ford made his final offer in Nov 2019. Between May 1, 2020, and April 30, 2023, Ford will pay 1% and not a penny more (Bill 124).
Some think this fair, but does it even make sense?
In 2020, gas was $1.04 per litre. Today, it is $1.70, in S. Ontario. Government wants to fill the medical gas tank at $1.04, plus 1 per cent per year.
Health Reform on the Fly
The proposed contract has far too many silly details to unpack them all: arbitrary limits to practice size, micro-managing office locations, and more. Each detail requires several paragraphs to unpack.
Consider one example.
In the late 1990s, family doctors were a dying breed. Medical students avoided family medicine, and nearly 1.5 million Ontarians could not find a family doc.
Government absolutely refused to increase fees for GP services. Fee for service (FFS) medicine rewards doctors for meeting as many patient needs as possible. It offers no easy way to contain spending.
In the early 2000s, government agreed to increase payments to primary care, but only if government could gain control of costs.
Primary care reform offered the answer.
A basket of patient-enrolment models (FHNs, FHGs, and FHOs) incentivized doctors to roster patients in return for an annual fee. The top rates for an average patient run around $200 per year, to provide a basket of approximately 130 services.
Very few family docs practice FFS medicine any more, although most specialists still do. FFS is bad, according to the experts. It rewards doctors for providing more services. More services mean the government must spend more on care.
Rostered, patient-enrolment models encourage doctors to offer fewer, longer visits, instead of churning patients for multiple return visits. Rostering incentivizes team care and coming up with creative ways to interact and share information without dragging patients back to clinic.
Whereas FFS incentivizes increased visits, rostering is designed to decrease them.
Government has decided it does not like fewer visits after all.
The Ministry of Health wants FFS visit numbers with rostered-payment certainty. Government aspires to 88 visits per week for every 1300 patients rostered. This will incentivize more frequent, shorter visits. It is hard to see how chopping one long visit into three in order to meet government targets will improve quality or care.
How Should You Vote?
It’s not a great offer. But at least it’s only 3 years.
This comes from the OMA negotiations team, in a town hall meeting. It is almost verbatim.
Better accept this offer or else. There is no guarantee of getting half as good at arbitration.
A Hobson’s choice is one which does not offer an alternative: take it or leave it. Unpalatability of the alternative removes real choice.
Closing Thought – Incomes as Information
“Doctors earn enough.”
“You can take the cut.”
I have heard many variations of this modern noblesse oblige. The average doctor lives well enough.
As a physician, you care about your income. It matters to you and your family. But that is not why your income matters to the rest of the world.
Physician income only matters to the extent it impacts patient care.
Does your income attract others to train in your specialty? Do your fees reward you for taking extra call each month?
We want the world to think we would do extra call for free. But it is not true. If people are not paid properly, call schedules become impossible to fill. Emergency departments become short staffed.
I need solid fees in place to guarantee that a vascular surgeon has moved to our area and is eager to answer my call at 3 in the morning. If I have no vascular surgeon, my patient dies.
The PPSA is not about you as a doctor. It’s about whether it is good for patient care.
Does the PPSA build healthcare?
Will your PPSA vote increase care overall or will it undermine the frail shell we have currently?
I cannot in good conscience support this contract. In this PPSA vote, I will vote no.
Photo credit: Pixabay Images Tumisu
Check out Part I: Doctors’ Contracts Are About Central Planning, Not Incomes: Ontario’s PPSA and all the excellent comments!

Thanks for the article Shawn. As an ophthalmologist I am looked at as a fat cat. Relativity makes my fee increase to .5%.
Throughout this pandemic I have been seeing patients face to face 6 inches away. Obviously surgery and elective office exams were deferred or cancelled. Could not make that up by calling patients and asking them to put their eyes up to the phone so I could examine them. No blood work to review online just one way to keep patients sight; in person.
Watching the agreement so out of step with inflation is just another kick in the teeth. Raising minimum wage means my staff need to be increased a significant amount in order to make sure they don’t fall behind.
This deal does nothing for me but as usual the OMA has failed with its negotiations for all MDs. I remember as a newly minted md going to one of the dog and pony shows of the OMA presenting their deal. They didn’t even try to sell it as a good deal. They just said it could have been worse. Their excuse was they’re going to the table with an empty gun. Now it’s even worse. They have sold any attempts to negotiate in order to maintain their exclusive representation rights.
It will eventually come home to roost as more and more MDs see the writing on the wall.
Brad
Hey Brad,
Thanks for sharing this. I had not even considered the virtual visits, bloodwork, and face-to-face issues for your specialty. In an overhead intense specialty like ophtho, I can only imagine what this will do to your net.
But as you say, people only see you with envy. In fact, envy is now promoted as a virtue — justice!
No one wins if we take our eyes off patients and start fighting each other about fees. How does this impact patients? Can I get ahold of an ophthalmologist when I’m worried about an eye injury? To be clear, I think the fee schedule needs an overhaul. But fighting like rats on a listing vessel is not the same as a thoughtful overhaul.
Really appreciate you taking time to read and post a comment!
Take care,
Shawn
Once upon a time, a long time ago , Ontario had Medical societies that sent delegates to Council , there was a time ( before my time …I used to have the minutes of our society , when I was a Treasurer, VP and President in rotation for over 14 years , off and on) when the medical societies themselves settled fees in their regions .
Medical societies held social functions, dinners, balls , lectures where doctors and spouses interacted…the delegates went to Council with their fingers on the pulse of the Societies that that they represented.
The highlight for me was my first attendance at Council in 1982 ( I think) …the OMA had gonads in those days and hired Ben Trevino, “ the best bloody labour relations lawyer in Canada”…he had won a 40% wage settlement in BC, a 20% wage settlement in Saskatchewan …” my own sense that the doctors will have to get much more angry than they are to consider a full strike as a remote possibility”( Trevino) .
Trevino whipped us up and we stood on the chairs punching the air…we went on strike and we won.
Foolishly , about 4 years later, without Trevino in the picture, the OMA thought that they could carry out the same strategy a second time, the same script, by that time the government had managed to entice/ seduce members of our profession , learned of our plans and prepared a strategy to counter it.
We failed, and, from my perspective , the profession never recovered its mojo….the OMA was outmanoeuvred in 2012 and it looks as if the coup de gras is going to be delivered if the profession votes yes in 2022.
A profession is finished when it begins to revere the chains that it helped the ministry to design.
Fantastic — thanks for sharing this, Andris.
I’ve heard snippets of those days. But few people take the time to share it … perhaps they cannot remember. The old local society structure thrived because docs needed it — it was crucial for referrals, coverage, consultations, help, etc. Not so anymore. Just send your patient to the hospital where someone you’ve never met will care for them.
I agree. Many doctors (especially from downtown Toronto) seemed to feel ashamed of 1986 for 30 years and longer. They could not separate their own income from the impact on patients.
Once professionals lose confidence in their own legitimacy, they can be ignored, manipulated, and hardly given a second thought.
The OMA should pay attention. Doctors will turn on it. A $100 million monopoly cannot survive unchallenged forever.
Thanks again!
I’m not familiar with how arbitration should work, but I smell a rat when the lead mediator is also the arbitrator. No set of fresh eyes or different perspectives offered. If there’s any bias with the mediator, that becomes reinforced with arbitration. Yes, judges should be fair and impartial. Maybe there’s benefit in not needing to repeat any learning curves about the issues discussed, as those have been hashed out in their entirety already. BUT, is there any pro government sentiment, any social justice consideration, any pro small business feelings??? I just don’t know…
We, as docs, are usually fairly independent, type A, solution oriented individuals. We want to get the work done and be efficient in doing it. We don’t want someone else to tell is how to do our jobs. Try telling your dentist or plumber how to drill or where to plunge. I don’t know if the arbitrator favours this direction for healthcare or has a different view should we present a fees only perspective. Does the arbitrator feel health care and docs need to be managed?
And can we trust OMA to present a hard NO to managed care and the metrics of control should this go to arbitration? The answer to that question would show us the real character of the OMA and that is one question I haven’t seen answered..
Fantastic questions, Rob!!
Exactly right. Although I believe the transition from mediator to chair of arbitration is legitimate, I share your worries about assumptions and biases. Labour lawyers are labour guys. I bugged them about this from the start. They have deep, deep connections within the Big Labour movement. They are not business guys.
Having said that, they hate losing! And they are smart. And they are experienced. What they need is a strong board of directors who can hold the lawyers on task. I worry that the OMA board swings hard left most of the time, until it gets taken over by a small group of frustrated docs … who are usually pro-business in an intuitive way (not philosophically conservative, by any means … just pro-small business).
Loved your analogies about where to drill or plunge. That is EXACTLY what I’ve been trying to get at. That sense is too often seen as heretical in medicine. We are just one member on the team, and a rather low member at that.
As always, sure appreciate your insight. People read through the comments! They love them. So thanks for taking time to share.
Cheers
Spot on as usual my friend. However I’m out of the fight this time. The CPSO made sure of that last time. But then again we have always been our own worst enemies.
I still recall one meeting where a family Doc derided the incomes of the ophthalmologist clan. My response was “we should be brought up to their level rather than bring them down to ours”
The look alone could have clogged a coronary.
Alas the good old days are gone and the new reality set in motion with the last battle will play out. I have no more fight. And at least my potty mouth will stay shut ;0)
Ozzy, you nailed it.
Raise everyone up. This pulls us together. Division drives everything down.
You fought well … I suspect you will continue to speak up, just in ways that can’t be caught in the media. 😉
Great to hear from you! Thanks again for all you do.
I have said many times over the last number of years,that the only way out now is radical system reform.I know you have written of this Sean.Things must get bad enough that the public will demand radical change. There are some hints with the OMA’s plan to expand surgicentres,anticipating the surgical backlog after the pandemic.Docs have been holding up the care/system for years trying to treat patients….they must/will let their arms fall to their sides in the interests of their own well being.Whether this PPSA passes or gets arbitrated,docs will remain collateral damage in a transition to something else.Therefore,docs must do whatever they must on an individual level to improve their quality if life,understanding the earnings hit they will continue to take in the near future.Nobless oblige is over and the patient is now each doc and their family.Quality/access will plummet,minor tasks will get farmed out further to pharmacists/NP’s/midwives, there will be another crisis in family medicine.Private alternatives will multiply….the Medicans/Cleveland clinics are thriving.Until we get enough alternatives to compete with our behemoth dinosaur of a system,there will be no incentive for govt to treat docs fairly…..none.The OMA knows this.Therefore the OMA serves no purpose,and should be rejected out of hand.They are just another cost on the backs of hard working docs .
Ram,
You are right, of course. I noticed the surgicentre stuff also. Hard to know how much Ford will do with it. Even if he does, government will still try to run it like it’s their own. Until we get the governance sorted out, we will keep having governance chaos.
Doctors haven’t realized that their monopoly on medicine isn’t what it used to be. It has been diluted and chopped in half, and half again. Scopes of practice have ballooned for everyone else, but doctors live in an even MORE rigid approach to scope of practice. The college and the government hate it when docs decide to branch out and try new things. Stay in your lane!
It’s hard to dwell on it too much. There is a better way. We need to focus on that.
Thanks again!
I write this as an actuary and as the father of two children currently doing their medical residency in Ontario. I have skin-in-the-game.
In September 2013, a colleague of mine at the Canadian Institute of Actuaries published a paper on the Sustainability of the Health Care System in Canada and its findings were as follows:
1) Assuming no governmental steps to curb health care expenditures, provincial/territorial spending
on health care is estimated to increase at 5.1 percent real growth per year, increasing from 44
percent today to 103 percent of total provincial/territorial revenues by 2037.
2) Even after assuming some governmental action to limit
real growth rates to 3.5 percent—and thus to decrease 2037 health care expenditures by 30
percent—health care will still absorb 69 percent of total revenues available to provinces/territories
by 2037 (86 percent of own-source revenues).
3) The proposed changes to the CHT will impact total revenues available to provinces/territories,
reducing the federal government’s portion of provincial/territorial health care expenditures from
the current 21.0 percent to 14.3 percent by 2037.
4) The supply of physicians needs to increase by at least 46 percent over the next 25 years just to
keep up with increased demand for services as a result of aging and population growth.
These horrible projections are the results of unfavourable demographics and the abject failure of past and current governments to appropriately pre-fund future gaps between tax intake and health care expenditures. This is a textbook Ponzi scheme, which I note is a criminal offense in the non-government world.
Once again, the majority of physicians will have to depend on the some of their colleagues moving to the US to exacerbate the physician shortfall and thus make the government realize that its decisions cannot be made in a vacuum.
It’s also absolutely essential that physicians be allowed to offer their services privately.
Is the government aware of these projections? If so, is it simply engaging in another round of kicking the can down the road? The problem is that we are fast running out of road. And if not, I offer my services to the OMA to help them get the seriousness of the problem across to the government.
Hey Jacques
Great comments. Why the heck did you let your kids go into medicine? 😀 Just kidding. Kids do what they do.
Re health spending as a portion of tax revenue: just raise taxes! We are nowhere near the 99% inheritance taxes England achieved in the late 1970s. (I’m being sarcastic, of course)
The OMA will never speak for system change, only more of the same. It is against its best interest to challenge the status quo.
Thanks for sharing this!