Everyone knows Canadian healthcare cannot continue without significant change. No one debates the need for it.
Popular solutions include:
– Build a hybrid or blended system
– Pay doctors and nurses less; put them on salary
– Limit services provided
People Look at Two Things:
Inputs: funding, expenses, cost cutting, efficiency, policy change, contract negotiations, etc.
Outputs: quality, performance, results patients get from the system.
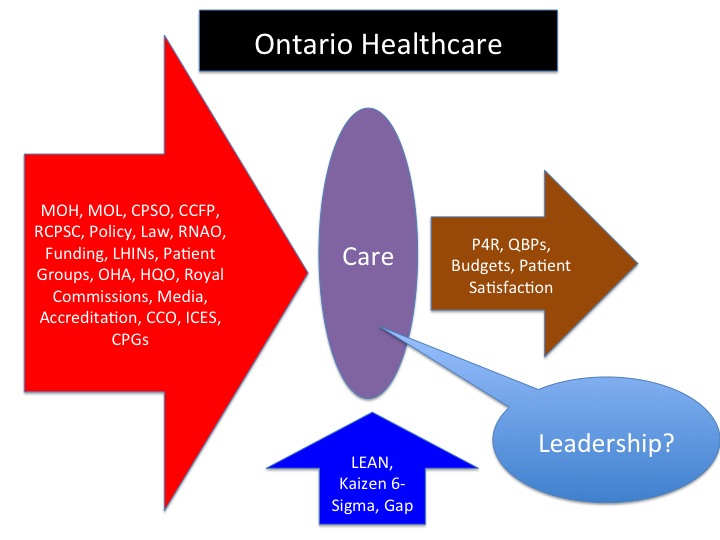
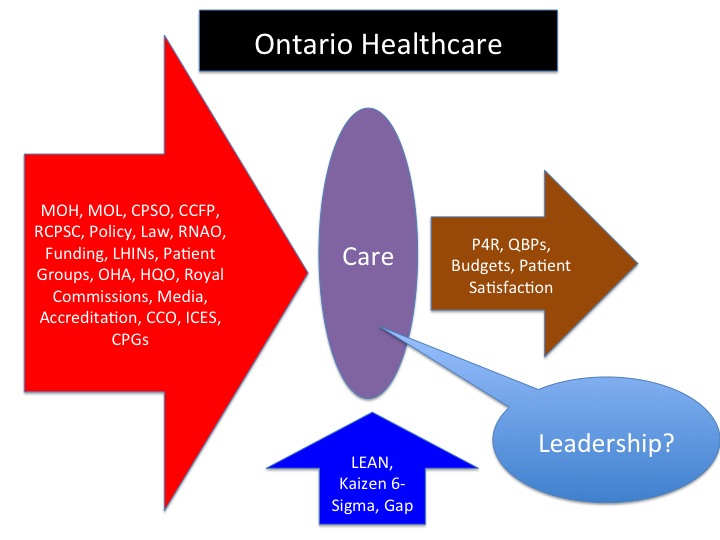
Inputs get most attention, but more sophisticated observers have started focussing on outputs. A few inside the system talk about ways to remove waste (LEAN, Gap analysis, etc.).
No one talks about control inside the system.
Funding Should Follow Governance
People make the imminent demise of our bloated healthcare system an issue of funding or spending, but it’s neither. Whether money comes from taxes collected by the government or ‘taxes’ collected by insurance companies, the issue is not about money.
The debate must shift from how money comes in to who’s in control of how money gets spent.
Everyone demands accountability from the system, but no one gives those in the system the freedom or authority to truly change outcomes. There are too many self-interested outside stakeholders trying to control the system all at the same time. They all think they know what’s best for patient care, but very few actually provide care.
Authorities make major decisions outside the system and then expect those within the system to operate after all the rules have been set; all the room to lead has been removed.
For example: the government negotiates contracts with nurses and then tells hospitals to be accountable to quality and efficiency within a contract that has zero productivity incentive.
We can still rescue publicly funded healthcare if we look at pockets of innovation where providers are given the chance to structure creative incentives that encourage clinicians to work differently.
We need to give the professionals inside the system a chance to show what can be done to improve patient access, quality, and service. You can’t demand accountability without giving people freedom to control and deliver what’s being asked of them.
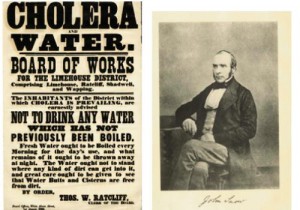 Nearly 2,000 people died of cholera in London, 1848. Those who survived boarded their apartments and fled to the countryside. Streets were bleached and sprinkled with sulfur to combat the foul odours, miasma, that experts believed caused the infection.
Nearly 2,000 people died of cholera in London, 1848. Those who survived boarded their apartments and fled to the countryside. Streets were bleached and sprinkled with sulfur to combat the foul odours, miasma, that experts believed caused the infection.