Medical students learn to despise paternalism. Patients must be given all information and helped to make their own decisions. It is better to cause pain and suffering with brutal honesty and unfettered autonomy than to presume benefit on a patient’s behalf. Students are taught that physicians must never bias patients in any way.
Medical students learn to despise paternalism. Patients must be given all information and helped to make their own decisions. It is better to cause pain and suffering with brutal honesty and unfettered autonomy than to presume benefit on a patient’s behalf. Students are taught that physicians must never bias patients in any way.
- What about depressed, suicidal patients?
- People who want to stop medications they need?
- Demented patients who won’t eat?
- Homeless people who won’t come in from the cold?
- Diabetics who won’t comply with treatment?
Should physicians be paid more when patients make healthy decisions? Should the outcome of patients’ decisions determine physician payment?
Paternalism
Refers to the limitations of personal liberty/freedom for an individual’s own good by the state, an organization, or other individual (Wikipedia and Stanford Phil).
- Soft versus Hard – Soft paternalism supports intervention when decisions are not truly voluntary (e.g. person does not understand a poison label). Hard intervenes even when people know what they are doing (e.g. suicide).
- Broad versus Narrow – Narrow relates only to concerns about state paternalism.
- Weak versus Strong – Weak paternalism interferes with freedom to promote an end valued by the individual (e.g., seatbelts; most people value safety). Strong interferes when an individual’s values are suspect (e.g., motorcycle helmet laws).
- Pure versus Impure – Impure paternalism changes a whole system to benefit a group (e.g. preventing cigarette manufacturing).
- Moral versus welfare – Welfare paternalism benefits health/safety only.
Should we force people to live healthy, safe lives?
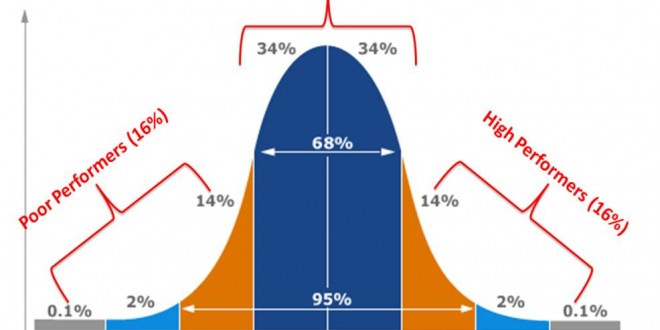
Physicians get bonuses based on how many of their patients get flu shots, mammograms, and other screening tests. Definitions and explanations can steer patients, while giving the impression of free decision making.
- Should patients be informed that physicians get rewarded for specific outcomes?
- Would it call into question the physician’s advice?
- Is this paternalistic?
Medicare provides, rations, and decides service based on beliefs about need/benefit. Medicare is paternalistic. Where do we draw the line between supporting state paternalism and opposing individual paternalism?
Please share your thoughts below!
(photo credit: wired.com)