
Everyone knows what it feels like to be a doctor. No, everyone hasn’t drilled holes into peoples heads or drained pus from buttocks. But every single person has experienced why doctors feel stressed.
Doctors spend their lives trying to offer less to people who want more. It’s like talking with someone who does not want to hang up the phone. All. Day. Long.
To be clear, it is not because doctors want to hang up. No, most doctors would love to talk forever, if we could afford it.
We like people.
Patient stories fascinate us.
But the clock ticks. Each minute means more overhead, with less to pay for it. Moments mean money that patients experience for ‘free’ and doctors experience as smaller payments to pay bigger bills.
Five dollars a minute. Patients get it for nothing. After the first 6-10 minutes for regular visits, doctors pay for the extra time.
Lopsided Relationship
This artificial everything-for-free arrangement sets up medicine as an unbalanced caller scenario. One person wants to stay on the call forever. The other person feels pressure to get off as soon as possible. Only politeness keeps us on the phone.
Doctors want to talk. And they do not want to go broke talking. Why can’t we find a way to let people talk as long as they want and pay for the experience, if they want it?
I know some patients would love it. And many doctors would love it too. A match made in heaven: Talkative patient meets sympathetic doctor. Talk away. Solve the world’s problems.
But the quants won’t allow it. You must stop talking. Stop listening!
Government will only pay you $33 for a conversation, while $13 goes to pay for the office and $19.80 goes to pay for the doctor’s salary, benefits, retirement, etc.
How much conversation can you buy for $20?
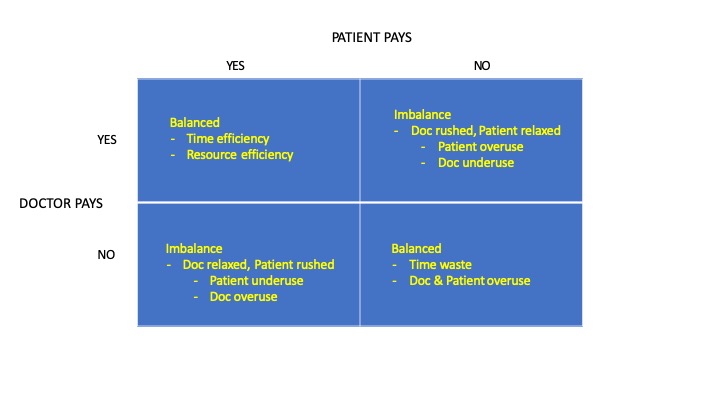
We have four options to pay for doctors, but Canada insists on choosing one that creates the unbalance of the top right box:
Arbitrary Imbalance
Pundits who watch medicine worry about physician burnout.
Why can’t doctors be happier?
What’s the problem with doctors?
Why won’t they just start being happy and thankful for the wonderful privilege they have to care for people in pain, fear, and distress?
Yes, doctors see doctoring as an enormous privilege. But how would you feel on a call from a distressed friend while you scurry to take your kids to parent-teacher interviews? If your whole career was spent in this emotional frame of mind, might you feel worn down eventually?
But doctors chose this career. Yes, we did.
But we did not choose arbitrary constraints on how much care we can offer.
Outrageous Solution
We need a system where the government provides, let’s say, 10 minutes. Or maybe 6 minutes. I’d prefer that government paid for 20 minutes for each patient, but government cannot afford it.
Then, if patients want more, they can pay for it. If they want 20 minutes or 30, they can pay for it.
<Gasp!>
But rich people would get more time! Poor people would get only 10 minutes!
This is not quite true.
If you wanted to forgo a colour TV to talk with your doctor, then you could choose.
But right now, the free-for-everything approach is killing doctors. It is killing compassion. It forces doctors to cut conversations short, when we really would love to talk as long as patients want.
So until we rearrange the alternate reality of artificial constraints placed on the doctor-patient relationship, doctors will continue to burn out, and patients will continue to feel rushed through the clinic.
Imbalance leaves both parties unfulfilled. We should change, not because it would make doctors feel better, but because patients would.
Photo credit: Pixabay Joffi and Pixabay NDE


We should be allowed to tell patients that ohip pays for one issue and we cannot charge for issues two three and four but we also cannot provide them for free. Right now we are all so afraid of college complaints that we cannot dare tell patients the truth! Just allow us to bill for extra problems and everyone will be happy.
Great solution, Jodie. The college/planners/overseers like it when we are too scared to speak up. So we try to cut patient visits as short as possible, when both we and the patients would love to have more time.
Thanks so much for posting!
In an APP model you could spend as much time as you want with each patient and not worry about who is paying.
It’s the FFS model, not the government, that is the problem.
Ok the government is a problem too, but that’s a whole other issue.
Thanks Hal!
Loved your comment about government! (I imagine you offer it with a very large happy face.)
You refer to the bottom right corner of the 2 x 2 table. I agree, APP/salary offers a balance between doctor and patient. However, it means that both the doctor and the patient cares nothing about cost or productivity when the government picks up the whole tab.
But I agree, an underfunded FFS system, without any payment by patients, is the core problem.
Thanks so much for reading and posting a comment!
Cheers
I just received from Dr. Brian Day his excellent editorial, “A constitutional solution for an ailing health system,” (BC Medical Journal, Jan/Feb 2020, page 5.)
He outlined several exempted groups such as those injured at work, federal employees, and federal prisoners. I would add, those who happen to live near an interprovincial border and can quite legally obtain a diagnostic procedure or surgery from a private facility in another province.
Let me give an example:
Several months ago, an American patient who has been a permanent visitor here for a number of years requested that I orfder an MRI from a private clinic in Quebec. She was seen on a Thurrsday, I obtained the requisition and faxed it, and she had the MRI across the Ottawa River in Gatineau the following day. The cost was $750. When I returned to my Appletree Clinic office the next Tuesday, to my pleasant surprise, the two- page report was in the EMR- in perfect English with no typos.
At the time I thought, while the Toronto Star and left-leaning people might consider it unfair that she could pay $750 for an MRI in one day rather than a “free” one at a hospital in a few months, how much do some people spend over a couple of months on their cigarettes, alcohol, and restaurant meals? Recall photos of Pearson airport at spring break, Christmas, etc. with a sea of humanity awaiting flights to Florida, Cuba, Mexico, etc. Many of these people are not “rich” but have different priorities for their disposable income than just their health.
Charles S. Shaver
Ottawa
Well said, Charles. Thanks for sharing this!
The Commonwealth Fund’s latest statistics reveal that Canada has only 2.7 MD’s per 1000 population , #10 out of 11…with Norway leading with 4.8 per 1000…beating out the USA at 2.6 :1000….Canadians are supposed to feel proud that Canada at least beat out the USA in this regard.
Canada and the USA, neither of which have world class health care systems, should stop comparing themselves to each other and avert their eyes to look abroad.
Canada’s total health care expenditure is #4 in the world beaten only by Australia ( with 3.5 MDs : 1000) Austria ( 5.14: 1000) and Belgium (3.32:1000) with the USA at #35 ( 2016).
The health care money expended in Canada is certainly not being spent on its “ lazy, greedy, selfish” medical profession…the cost of Canadian health care bureaucracy ( with their benefits and pensions) is certainly not languishing at #10.
The money is certainly being spent elsewhere.
The bloated overcompensated health care bureaucracies, with benefits and pensions , are making increasingly onerous and unrealistic demands of the undercompensated, benefitless and pensionless MDs struggling at the coal face, with no concept of their overheads and of their responsibilities in managing medical practices as they move the goal posts….increasingly reducing their incomes whilst jacking up their overheads even as they abuse them.
Young graduating doctors are being introduced to stress by the absurd matching process at the beginning of their careers…it only gets worse from there….how many Canadian MDs are languishing unmatched today? How many unemployed under employed specialists are there sitting on their hands?
Are they included in the Canadian 2.6 per 1000?
Stress is inherent and inevitable in the practice of medicine , governments and bureaucratic bright ideas such as matching compound them.
Always a solid comment, Andris.
The waste of bureaucracy is always justified as less expensive than the cost of ‘advertising’ in a free market approach. The fact that patients stand in line in the bureaucratic approach gets lost in the discussion.
Thanks again!
When I was much younger, I saw my doctor once a year for 5 minutes because I was healthy. Now that I’m
60 years old I have a lot of health issues that are developing so I see her a lot more often. I would restrict myself to one issue at a time but seeing as they are interrelated we end up talking about all of them. I am aware that OHIP only pays for 5 min appointments but what is a person supposed/allowed to do? It’s hard enough to get any appointment at all, I don’t know how successful I would be if I tried booking several appointments fairly close together. Is there a hybrid medical funding system anywhere in the world currently that serves both the paying and subsidized patients almost equally well ? I know that people in the UK can opt out of the NHS, but I’m not sure how that works and I don’t know anyone who lived/lives there
to ask. I have always felt that most doctors in Ontario are criminally underpaid, but I’ve never heard of any politician running on a platform of “let’s pay doctors what they’re really worth”. I enjoy reading your columns, thanks for letting regular folks read them.
Thanks for reading and taking time to share an excellent comment, Lily!
I am so glad that you even think about these things. Most people just plow through their list and get frustrated (usually politely) if they cannot complete it.
To be clear, there are fees that can justify a 20-30 minute visit. But they are allowed only under strict conditions. In addition, many doctors receive one fee to care for you all year (called capitation), for example, $140 no matter how many visits you require. This is great if you, as a doctor, have a huge number of people signed up who never need to see you. But if you have sick people — the ones who need care — you will go broke.
But this is getting off track. I was trying to focus on the arbitrary imbalance injected into the relationship. It works better if both parties want to do what is necessary but not spend any unnecessary time doing it. They should have aligned interests.
Thanks so much for your kind words. I’m glad you like the posts.
Cheers
The problem is that the population today is less healthy than it was decades ago when free Medicare was introduced. If we want to be able to avoid burn-out and begin to have a sustainable health care system (with benefits and pensions for MDs, I add), respective governments must start using public policy tools to encourage people to improve their lifestyles (which will address most chronic health issues), and they must change the remuneration model so that MDs can be paid appropriately for taking the time to outline the benefits of diet, exercise, adequate sleep, etc. Otherwise things will continue to spiral out of control and many will seek out more privately funded jobs to offset the losses experienced in the FFS / FHG etc models.
When the British National Health care system was imposed in 1948, Aneuryn Bevan having “ stuffed the mouths of the British Medical Association hierarchy with gold, honours, titles, sinecures” to betray future generations of British doctors …there was an initial injection of money into the health care system.
The idea was that having gone over the initial hump of backlogged hernias etc., that the British population would become so healthy that there would be less requirement for medical doctors etc., …so they started to cut back on training doctors in anticipation of a future healthy population requiring less medical services.
The NHS central planners and the political class got it completely wrong…the opposite happened….with prosperity and longevity came increased demand and cost…£150 Billion 60 years ago ..x 10 today….ER’s are overwhelmed…life expectancy increased as infectious diseases became less of a problem ( of course the threat of viral pandemics ever remain as we see today) , fewer are dying of MIs , Cancer sufferers are living longer…chronic CVS diseases, diabetes and dementias are surging …by 65 most will have one of the three…by 75 two.
A 65 year old costs x2.5 that of a 30 year old…an 85 year old x 5.
The British NHS has an increasing shortage of hospital beds, nurses, doctors…there is a shortage of FPS with trainee positions remaining empty….Brexit, with the exit of EU nurses and doctors, will be compounding NHS’s problems.
The British NHS is Canada’s health care system’s ideological mothership and we are tracking its path…it is unsustainable in Canada which does not have the free market safety valve that the world class symbiotic hybrid public private health care systems possess….scapegoated Canadian doctors’ incomes will be squeezed more and more and governmental oppressiveness will increase and increase , making entry into the medical profession in Canada less and less attractive, until the final collapse.
Great comments from both of you, Jennifer and Andris (again!).
I agree that older people have more complex problems. The “preventative care” that Tommy Douglas believed in has not delivered the grand saving that he and his cohort promised. If anything, it has delivered the opposite.
So part of me worries, Jennifer, about putting too much weight on patient behaviour. Having said that, I am in full agreement about discussing the demand side of the demand-supply equation when it comes to dangerous living or outright disdain for any sort of healthy living followed by demands for care. My grandparents seemed to spend more time worrying about maintaining their health to avoid the cost of a visit for medical attention.
“Stuffing their mouths with gold” works every time, for every project, and every constituency. It is the wide road to destruction for democracies.
Thanks again to both of you!
Cheers
Jennifer – great to see we both read Shawn’s writing.
I look forward to debating with you in the next election!
Good post Shawn.
My thoughts on this topic,specifically,physician burnout/happiness are well known to you……CHOICE.
Physicians,by nature,are hard working independent thinkers who,like patients require the ability to CHOOSE ….. how they are paid,how much money they want to make,how many patients they want to see,how long they spend with each patient,how/what they want to practise,where they want to practise,and whether or not they want to belong to a medical association (OMA).
Increasingly,that choice has been taken away from med students (matching)to practising physicians ….. causing more and more stress/unhappiness.It’s quite simple,really …. it’s what I call the ‘human condition’.
As a ‘self help’ group,we should start taking control by making membership in the OMA voluntary, which would start the ball rolling while we wait for Dr Day’s court decision and the Charter challege(why is the OMA dragging its feet on this ?).
Great comments, Ram
1. Quality by committee will never match the quality that emerges from choice. And I agree with your call for choice in all things.
2. I mentioned this on Facebook: Collective action works when small, aligned groups advance a single message. This comes from Mancur Olsen’s The Logic of Collective Action, 1971 (on my reading list). We need to ask, “At what point is a group too big and too diverse to be able to create a uniform message?” We saw how powerful the OBs were in the late 1990s over CMPA fees. They had one message, and they all supported the plan of action. Can 31,000 practicing docs develop one message, backed by one plan of action, that all members will support? This is a very hard thing indeed!
3. As for the OMA, and all other associations, being silent on the lawsuit regarding whether Canadian citizens have the right to purchase medically necessary care when wait times in the public system grow too long, well, I think this is an oversight. It is divisive, but we should have an opinion. I think both ends of the spectrum are too scared that the opposite end will hi-jack the program. And those in the middle are too scared to be attacked by zealots at either end.
Again, thanks so much for reading and posting a comment! I’ve been too busy this month trying to tie up loose ends for a sabbatical in March and April. Should have more time to write then (I hope).
Talk soon,
S